Most people don’t think about their kidneys until something goes wrong. But when a common medication like omeprazole or ibuprofen triggers a hidden kidney reaction, the damage can sneak up fast. Acute interstitial nephritis (AIN) is one of those silent threats - a sudden inflammation in the kidney’s filtering tissue caused mostly by drugs. It’s not rare. In fact, it’s responsible for up to 15% of all sudden kidney failures in hospitals. And the number of cases is rising, especially as more people take proton pump inhibitors (PPIs) for heartburn.
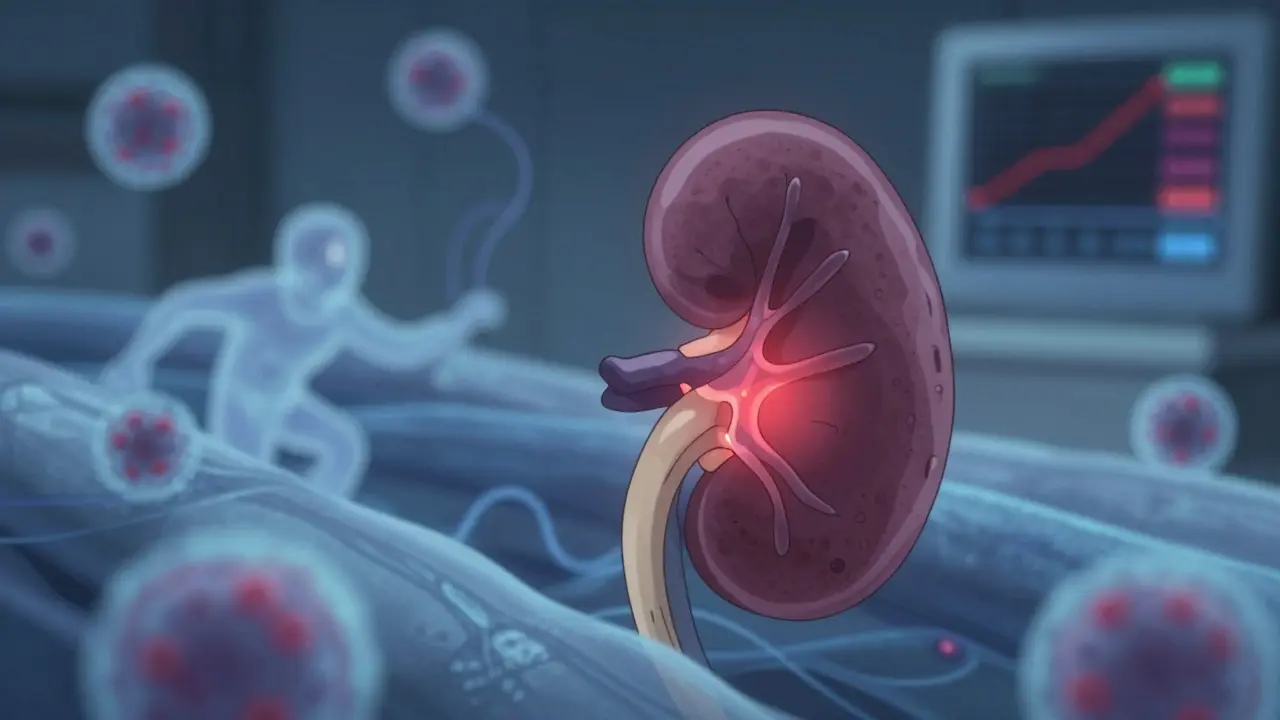
What Actually Happens in Your Kidneys When AIN Strikes
Your kidneys are made of millions of tiny filters called nephrons. Between these filters is the interstitium - a space filled with connective tissue and immune cells. When a drug triggers an allergic-type reaction, your body sends immune cells into this space. They swell up, leak fluid, and start attacking the tubules that help clean your blood. This isn’t an infection. It’s your own immune system going rogue.
The classic signs - fever, rash, and eosinophils in the blood - show up in fewer than 10% of cases. That’s why most people get misdiagnosed. They think it’s a urinary tract infection or just feeling off. But the real clues are subtle: a drop in urine output, unexplained fatigue, nausea, or a sudden rise in creatinine levels during a routine blood test. These aren’t dramatic. They’re quiet. And that’s what makes AIN so dangerous.
The Top 3 Drug Culprits Behind AIN
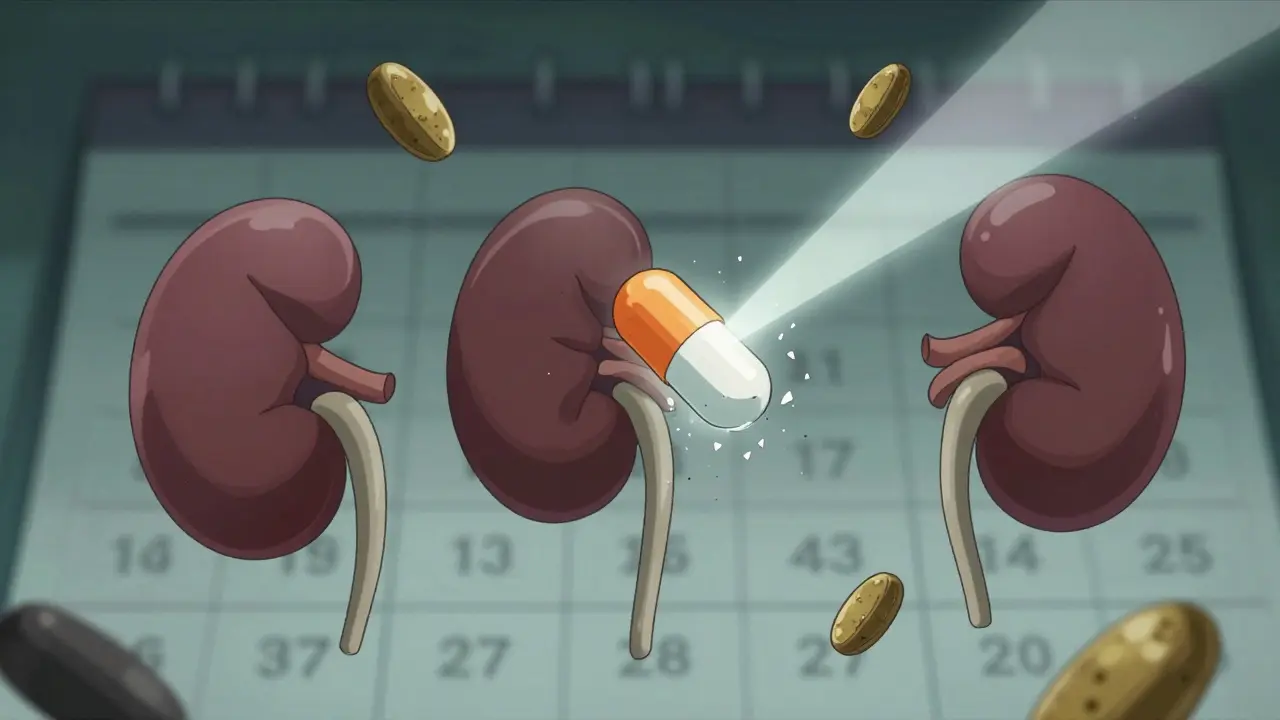
Over 250 medications have been linked to AIN. But three classes dominate the list:
- Proton pump inhibitors (PPIs) - like omeprazole, pantoprazole, esomeprazole. These are the fastest-growing cause. Once considered safe, they now account for nearly 4 out of 10 AIN cases. People often take them for months or years, thinking they’re harmless. But the damage builds slowly. Recovery is slower too - only half of patients get back to full kidney function.
- Antibiotics - especially penicillins, cephalosporins, and sulfonamides. These cause about 30% of cases. They tend to strike faster - within days, not months. You might get a rash or fever, which helps clue doctors in. But even then, diagnosis is often delayed.
- NSAIDs - ibuprofen, naproxen, diclofenac. These make up nearly half of all drug-induced AIN cases. They’re especially risky for older adults or those with existing kidney issues. Unlike antibiotics, NSAID-induced AIN rarely causes a rash or fever. Instead, it often shows up as heavy proteinuria - more than 3 grams of protein in the urine per day. That’s a red flag.
Here’s what the data shows about recovery by drug type:
| Drug Class | Recovery Rate | Median Recovery Time | Chronic Kidney Disease Risk |
|---|---|---|---|
| Antibiotics | 70-80% | 14 days | 20% |
| NSAIDs | 50-60% | 28 days | 42% |
| PPIs | 50-60% | 35 days | 35% |
Notice something? The drugs that cause the most cases - PPIs and NSAIDs - are also the ones with the worst recovery odds. And the longer you take them, the higher your risk.
Why Diagnosis Is So Often Delayed
Patients often wait 2 to 4 weeks before getting the right diagnosis. Why? Because the symptoms mimic other problems. A dull backache? Maybe it’s a muscle strain. Feeling tired and nauseous? Stress or the flu. A slight drop in kidney function? Maybe just dehydration.
Doctors don’t automatically think of AIN unless they’re told the patient is on a known trigger drug. And many patients don’t even realize their heartburn pill or painkiller could be the culprit. A 63-year-old woman in a documented case took omeprazole for 18 months before her kidneys started failing. She needed dialysis for three weeks. Even after recovery, her kidney function never fully returned - her eGFR stayed at 45, down from 85.
There’s no simple blood test or urine dipstick that confirms AIN. The only sure way is a kidney biopsy. That’s a big hurdle. Many patients and doctors hesitate. But without it, you’re guessing. And guessing costs time. And time is what you don’t have when your kidneys are shutting down.
What Happens After You Stop the Drug
Stopping the offending drug is the single most important step. In fact, the American Society of Nephrology says it’s the cornerstone of treatment. If you catch it early - within a week of symptoms - your chances of full recovery jump by 35%.
Most people start feeling better within 72 hours of stopping the drug. One Medscape survey of 120 patients found 65% improved in just three days. But improvement doesn’t mean recovery. Your kidneys can still be damaged underneath.
For severe cases - where eGFR drops below 30 - doctors often turn to steroids. Prednisone or methylprednisolone is given for 2-4 weeks, then slowly tapered over 6-8 weeks. The evidence isn’t perfect. There are no big randomized trials proving steroids work. But experts agree: when kidney function is crashing, steroids can help. Dr. Ronald J. Falk from UNC Kidney Center says, "If you wait too long, the damage becomes permanent. Steroids aren’t magic, but they’re often the best shot you’ve got."
Not everyone needs them. If your kidneys are only mildly affected and you stop the drug fast, you might heal on your own. But if you’re on dialysis, you’re in the danger zone. About 15-20% of AIN cases need temporary dialysis. Most get off it within 2-6 weeks. But for some, it’s the beginning of long-term kidney disease.
Who’s Most at Risk - And How to Protect Yourself
You’re at higher risk if:
- You’re over 65
- You take 5 or more medications regularly
- You’ve had kidney issues before
- You’re on PPIs for more than 3 months
- You take NSAIDs daily for pain or arthritis
People on multiple drugs have over 3 times the risk. That’s why polypharmacy is a silent killer in older adults. A 72-year-old taking omeprazole, lisinopril, atorvastatin, metformin, and ibuprofen is playing with fire.
Here’s what you can do:
- Ask your doctor: "Could any of my meds be harming my kidneys?" Especially if you’ve been on them for over a year.
- Get a basic kidney check - serum creatinine and eGFR - at least once a year if you’re over 60 or on chronic meds.
- Don’t take NSAIDs daily unless absolutely necessary. Try acetaminophen instead for pain.
- If you’ve been on a PPI for more than 3 months, ask if you still need it. Many people take them way longer than they should.
- Track your symptoms. Fatigue, nausea, swelling in ankles, or reduced urine output? Don’t brush it off. Get it checked.
What Recovery Really Means - And the Hidden Long-Term Risk
Many patients think "recovery" means they’re back to normal. But it’s not that simple. About 30% of people with AIN develop chronic kidney disease within a year. That’s stage 3 or worse - meaning permanent loss of kidney function.
NSAID users have the highest risk: 42% end up with long-term damage. PPI users aren’t far behind. Even if your creatinine levels drop back to normal, your kidneys might not be fully healed. Scar tissue can form in the interstitium. That’s invisible on blood tests. Only a biopsy shows it.
A 2022 study found that 42% of AIN patients still had eGFR below 60 at the 6-month mark. That’s not mild. That’s moderate kidney disease. And it’s preventable - if caught early.
The good news? If you stop the drug fast and get treatment early, most people avoid dialysis. The bad news? Many don’t. And the number of cases is rising. PPI use has grown by 27% since 2010. The FDA issued a warning in 2021 after over 1,200 cases were reported. By 2025, AIN cases could rise another 15% if nothing changes.
What’s Next? New Tools on the Horizon
Right now, we’re stuck relying on biopsies. But research is moving fast. A new biomarker - urinary CD163 - showed 89% accuracy in detecting AIN in a 2022 study. That could mean a simple urine test replacing a biopsy in the next few years.
Scientists are also looking at how immune checkpoint inhibitors - cancer drugs - trigger AIN. It’s a growing concern as more people get these treatments. And we’re starting to understand why some people are genetically more prone to drug reactions.
For now, the message is clear: don’t ignore subtle kidney symptoms. Don’t assume your meds are safe just because they’re over-the-counter. And if you’ve been on a PPI or NSAID for years - talk to your doctor. A simple blood test could save your kidneys.
Can acute interstitial nephritis be reversed?
Yes, if caught early. Stopping the triggering drug within the first week gives you a 70-80% chance of full kidney recovery. But if diagnosis is delayed beyond 14 days, the chance of complete recovery drops sharply. Some damage can become permanent, especially with NSAIDs or long-term PPI use.
Which drugs are most likely to cause acute interstitial nephritis?
The top three are proton pump inhibitors (like omeprazole), antibiotics (especially penicillins and sulfonamides), and NSAIDs (like ibuprofen and naproxen). PPIs are now the second most common cause, after NSAIDs, and their use has grown sharply over the last decade.
Do I need a kidney biopsy to diagnose AIN?
Yes. While blood and urine tests can suggest AIN, only a kidney biopsy can confirm it. Other tests like eosinophiluria or gallium scans are unreliable. If your doctor suspects AIN and your kidney function is declining, a biopsy is the only way to know for sure - and to rule out other serious conditions.
How long does it take to recover from drug-induced AIN?
Recovery time depends on the drug. Antibiotic-induced AIN usually improves in about 14 days. NSAID-induced cases take around 28 days. PPI-induced AIN often takes 35 days or longer. Improvement often starts within 72 hours of stopping the drug, but full recovery can take weeks to months. Some people never fully regain their original kidney function.
Can I take NSAIDs again after having AIN?
No. If you’ve had AIN from an NSAID, you should avoid all NSAIDs permanently. Re-exposure can trigger another episode - often more severe. Even a single dose can cause a relapse. Talk to your doctor about safer pain relief options like acetaminophen.
Is acute interstitial nephritis common?
It’s not rare - it causes 5-15% of all acute kidney injuries in hospitals. Drug-induced AIN alone affects about 12 out of every 100,000 people each year. That number is rising, especially in older adults and those on long-term medications like PPIs. It’s one of the most preventable causes of kidney damage.
What to Do Now
If you’re on a PPI, NSAID, or antibiotic long-term, don’t panic. But do act. Ask your doctor for a basic kidney function test - serum creatinine and eGFR. If you’ve had unexplained fatigue, nausea, or swelling in your legs, mention it. If you’ve had AIN before, keep a list of all your meds and share it with every new doctor. Your kidneys can’t tell you they’re hurting. You have to speak up for them.

Comments
Skye Kooyman January 27, 2026 AT 21:40
Been on omeprazole for 5 years. Never thought it could do this. Got my creatinine checked last week. Still normal. But now I'm scared to stop.
Suresh Kumar Govindan January 28, 2026 AT 17:03
The pharmaceutical-industrial complex has weaponized heartburn. PPIs are not medicine. They are corporate sedatives for the modern digestive malaise. You do not need them. You have been conditioned to believe you do. Your kidneys are paying the price for your convenience.
James Nicoll January 30, 2026 AT 16:10
So we’re telling people to stop taking ibuprofen because some guy in a lab got a weird rash? Meanwhile, my grandpa takes two Advil a day for his knees and still hikes every Sunday. Maybe the real problem is overmedicating the healthy and undermedicating the dying. Also, who wrote this? A nephrologist or a TED Talk ghostwriter?
Aurelie L. February 1, 2026 AT 10:56
My sister got dialysis after 18 months of omeprazole. They didn’t catch it until her hands swelled up like balloons. Now she’s on a 20-pill-a-day regimen. No one warned her. No one even asked if she was taking heartburn meds. This isn’t medicine. It’s negligence dressed up as care.
Peter Sharplin February 2, 2026 AT 14:29
Important context: the 42% chronic kidney disease rate for NSAID-induced AIN is from a 2021 multicenter cohort study. But the real risk multiplier is polypharmacy - especially when combined with ACE inhibitors or diuretics. The biopsy gold standard remains, but emerging biomarkers like urinary CD163 are showing 89% specificity in early trials. If you're over 60 and on three or more meds, get a baseline eGFR and repeat every 6 months. Don’t wait for symptoms. They’re too late.
George Rahn February 3, 2026 AT 00:48
The American medical establishment has become a cathedral of bureaucratic inertia. We diagnose with biopsies because we fear liability, not because we understand biology. We prescribe PPIs like candy because insurance companies reward volume, not vigilance. And now we wonder why kidneys fail? It is not the drug. It is the system. The system that treats the body as a machine to be patched, not a living organism to be respected. The PPI is merely the symptom. The disease is our collective surrender to pharmaceutical dogma.
Kipper Pickens February 3, 2026 AT 15:39
For those asking about alternatives: magnesium oxide for heartburn, H2 blockers like famotidine for short-term relief, and lifestyle changes - no late meals, elevate the head of the bed, reduce caffeine and citrus. NSAID alternatives? Acetaminophen, physical therapy, topical capsaicin. The data supports it. The guidelines don’t always reflect it. But you can still ask. You should ask.
Uche Okoro February 4, 2026 AT 13:44
Re-exposure to NSAIDs post-AIN induces a T-cell-mediated hypersensitivity cascade with amplified interstitial fibrosis via IL-13 and TNF-alpha upregulation. The risk of recurrent injury is not merely elevated - it is biologically deterministic. Avoidance is not precautionary; it is existential. Your renal tubules are not a gamble. They are irreplaceable. The data is unequivocal. The clinical imperative is absolute. Do not test fate. Do not rationalize. Do not take the pill.