When a medication triggers a severe allergic reaction, time isn’t just money-it’s life. Anaphylaxis from medication doesn’t wait for a doctor’s appointment. It hits fast, often within minutes, and can shut down breathing, drop blood pressure, or stop the heart. This isn’t a mild rash or a stomach upset. This is a medical emergency that demands immediate, correct action. And the difference between life and death often comes down to whether someone knows exactly what to do-and does it without hesitation.
What Happens During a Medication-Induced Anaphylaxis?
Anaphylaxis from medication happens when your immune system overreacts to a drug, treating it like a dangerous invader. Common culprits include antibiotics like penicillin, NSAIDs like ibuprofen, chemotherapy drugs, contrast dyes used in imaging scans, and muscle relaxants given during surgery. About 20-30% of all hospital anaphylaxis cases come from medications, according to the Resuscitation Council UK. The reaction can strike even if you’ve taken the drug before without issue. One dose, and suddenly your body goes into full alarm mode.
Symptoms aren’t always obvious. Many people assume anaphylaxis means hives or swelling. But in 10-20% of cases, there’s no skin reaction at all. Instead, you might notice:
- Difficulty breathing, wheezing, or a persistent cough
- Swelling of the tongue, throat, or lips
- Hoarse voice or trouble talking
- Dizziness, fainting, or sudden collapse
- Pale, clammy skin-especially in children
These aren’t just uncomfortable symptoms. They’re signs your airway is closing and your blood pressure is crashing. Without quick intervention, this leads to cardiac arrest. The clock starts ticking the moment symptoms appear.
Step 1: Lay the Person Flat Immediately
One of the most dangerous mistakes anyone can make is letting the person stand, sit up, or walk around. That’s not just unhelpful-it’s deadly. Data from the Resuscitation Council UK shows that changing from lying down to standing triggers cardiovascular collapse in 15-20% of anaphylaxis cases. The body’s blood pressure drops so fast that standing can cause sudden death.
Here’s what to do instead:
- If the person is conscious and breathing, lay them flat on their back. Elevate their legs slightly if possible to help blood return to the heart.
- If they’re having trouble breathing, let them sit up with legs stretched out. Don’t force them flat if they can’t breathe that way.
- If they’re unconscious but breathing, place them in the recovery position-on their left side if they’re pregnant.
- For young children, hold them flat on your lap. Never hold them upright.
This positioning isn’t optional. It’s a critical part of keeping blood flowing to vital organs until help arrives.
Step 2: Administer Epinephrine Right Away
This is the single most important step. Epinephrine is the only treatment that reverses the life-threatening effects of anaphylaxis. Antihistamines like Benadryl? They help with itching or hives-but they do nothing for breathing or circulation problems. Corticosteroids? They may reduce delayed inflammation, but they don’t stop the immediate danger. Only epinephrine works fast enough.
Use an auto-injector: EpiPen, Auvi-Q, or Adrenaclick. Inject into the outer thigh-through clothing if needed. Hold the device in place for 10 seconds. The dose is 0.3 mg for adults and children over 30 kg. For children between 15-30 kg, use 0.15 mg.
Don’t wait. Don’t second-guess. Don’t look for a doctor. If you suspect anaphylaxis, give epinephrine. The Cleveland Clinic’s 2023 guidance states that epinephrine works in 1-5 minutes, but its effect lasts only 10-20 minutes. That’s why you still need emergency help even after giving it.
And here’s the hard truth: 70% of fatal anaphylaxis cases involve delayed or missed epinephrine. People wait for “clearer symptoms.” They fear side effects like a racing heart. But the data is clear: out of 35,000 epinephrine doses given for anaphylaxis between 2015 and 2020, only 0.03% caused serious heart problems. The risk of not acting is far greater.

Step 3: Call Emergency Services Immediately
After giving epinephrine, call 911-or your local emergency number-right away. Don’t wait to see if symptoms improve. Don’t assume the epinephrine fixed everything. The reaction can come back, sometimes stronger, hours later. This is called a biphasic reaction, and it happens in about 20% of cases.
Hospital observation is non-negotiable. The ASCIA guidelines require at least 4 hours of monitoring. For medication-induced anaphylaxis, newer data suggests a higher risk-up to 25% more likely than food-triggered cases. That’s why some hospitals now recommend 6-8 hours for these patients. Even if they feel fine after the first shot, they need to be watched.
Step 4: Give a Second Dose If Needed
Epinephrine doesn’t always work the first time. If symptoms don’t improve-or get worse-after 5 minutes, give a second dose. The Resuscitation Council UK and FAACT both recommend this. Some protocols allow doses every 10 minutes if symptoms persist.
People often hesitate to give a second dose because they think it’s dangerous. But in reality, the body needs more epinephrine to keep the airway open and blood pressure stable. If the first dose didn’t fully reverse the reaction, the second one could be lifesaving.
What Not to Do
There are common myths that cost lives:
- Don’t give antihistamines instead of epinephrine. They’re not a substitute. They’re for after the emergency is controlled.
- Don’t give oral medications. Swallowing pills or liquids is too slow when the airway is closing.
- Don’t wait to see if it gets worse. Anaphylaxis doesn’t wait. Neither should you.
- Don’t let the person drive themselves. Even if they feel okay, their condition can collapse without warning.
And here’s something most people don’t know: beta-blockers-commonly prescribed for high blood pressure or heart conditions-can make epinephrine less effective. If the person takes beta-blockers, they may need higher doses. This is especially important for adults over 40, since 25-30% of them are on these medications.
Why Do People Delay Treatment?
Even with clear guidelines, delays happen. A 2021 survey of 1,200 nurses found that 42% admitted waiting to give epinephrine because they were afraid of legal consequences or side effects. In outpatient settings, a FAACT survey showed that 68% of patients carry epinephrine auto-injectors, but only 41% feel confident using them.
Common mistakes during injection:
- Not holding the device in place long enough (37% of errors)
- Injecting into fat instead of muscle (18% of errors)
- Using the wrong dose for weight
That’s why newer devices like the Auvi-Q 4.0 include voice guidance. Clinical trials showed it improved correct use from 63% to 89% in untrained users. If you or someone you know has a medication allergy, practice with a trainer device. Know where the injection site is. Know how long to hold it. Don’t wait for an emergency to learn.
What Happens After the Emergency?
Once stabilized, the patient will need follow-up care. This includes:
- Referral to an allergist for testing to identify the trigger
- Prescription of two epinephrine auto-injectors (never just one)
- Education on avoiding the drug and reading medication labels
- Medical alert bracelet or card
Some medications have cross-reactivity. For example, if someone had anaphylaxis to penicillin, they may also react to similar antibiotics. A specialist can map out safe alternatives.
And while research continues-like the NIH’s 2023-2025 study on dosing by BMI instead of weight-the core message hasn’t changed: act fast, give epinephrine, call 911, stay for observation.
Final Thought: Hesitation Kills
There’s no such thing as being too cautious with anaphylaxis. The ASCIA First Aid Plan says it plainly: “IF IN DOUBT, GIVE ADRENALINE.” That’s not a suggestion. It’s a lifesaving rule backed by data from Australia, where hesitation caused 35% of preventable deaths between 2015 and 2020.
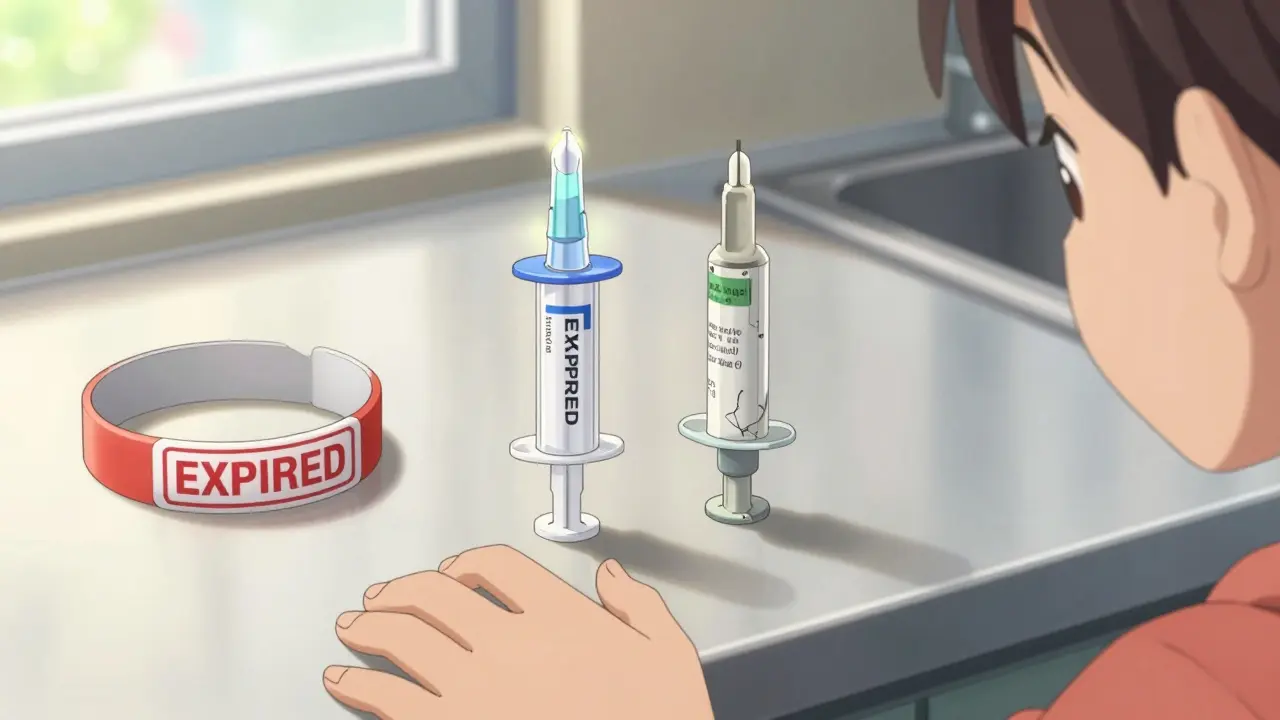
If you’re a parent, caregiver, or someone with a known drug allergy, keep your epinephrine with you at all times. Check the expiration date. Teach your family how to use it. Practice with a trainer. Make sure your workplace or school has a plan.
Anaphylaxis from medication doesn’t announce itself with warning signs. It strikes silently, quickly, and without mercy. But you can change the outcome. You just need to know what to do-and do it without waiting.
Can anaphylaxis happen even if I’ve taken the medication before without issues?
Yes. Anaphylaxis can develop after repeated exposure to a drug. Your immune system can become sensitized over time, meaning a reaction may occur on the second, third, or even tenth dose. Never assume past tolerance guarantees future safety.
Is it safe to use an epinephrine auto-injector if I’m not sure it’s anaphylaxis?
Yes. The risk of giving epinephrine when it’s not needed is extremely low. Side effects like a racing heart or nervousness are temporary and far less dangerous than untreated anaphylaxis. The guideline is clear: if you suspect anaphylaxis, give epinephrine. Don’t wait for perfect symptoms.
Why can’t I just give Benadryl instead of epinephrine?
Benadryl treats skin symptoms like itching or hives, but it does nothing to open airways, raise blood pressure, or prevent shock. In fact, relying on antihistamines alone delays life-saving treatment. Studies show no reduction in death rates when epinephrine is withheld. Epinephrine is the only treatment that reverses the core dangers of anaphylaxis.
How long should someone be monitored after an anaphylactic reaction?
At least 4 hours in a medical facility. For medication-induced anaphylaxis, experts now recommend 6-8 hours because the risk of a second reaction (biphasic reaction) is higher than with food triggers. Even if the person feels fine after epinephrine, they must be observed for signs of recurrence.
Can I use an expired epinephrine auto-injector?
If it’s the only option during an emergency, yes-use it. While potency may decrease after expiration, studies show many expired devices still deliver a meaningful dose. Don’t let an expired device become an excuse to delay treatment. Replace it as soon as possible after the emergency.
What should I do if the person becomes unconscious?
Lay them flat, call emergency services, and administer epinephrine if available. If they’re not breathing or have no pulse, begin CPR immediately. Epinephrine should still be given, even during CPR. Continue CPR until help arrives or the person shows signs of recovery.

