For decades, women have been told to use backup birth control when taking antibiotics. It’s been printed on pharmacy labels, repeated by well-meaning friends, and even suggested by some doctors. But here’s the truth: most antibiotics don’t interfere with birth control pills. The fear isn’t based on science-it’s based on a myth that won’t die.
Why the Myth Started
The story began in the 1970s when a few women on birth control got pregnant while taking antibiotics. At the time, researchers didn’t have the tools to figure out why. One case involved rifampin, a powerful antibiotic used to treat tuberculosis. That drug does interfere with hormonal contraception. But instead of isolating that one exception, the message got twisted: All antibiotics might lower birth control effectiveness. That idea stuck. Even though dozens of studies since then have shown otherwise, the warning still shows up on pill bottles and in pharmacy conversations. It’s easier to tell everyone to use condoms than to explain the difference between rifampin and amoxicillin.The Real Culprit: Rifampin and Rifabutin
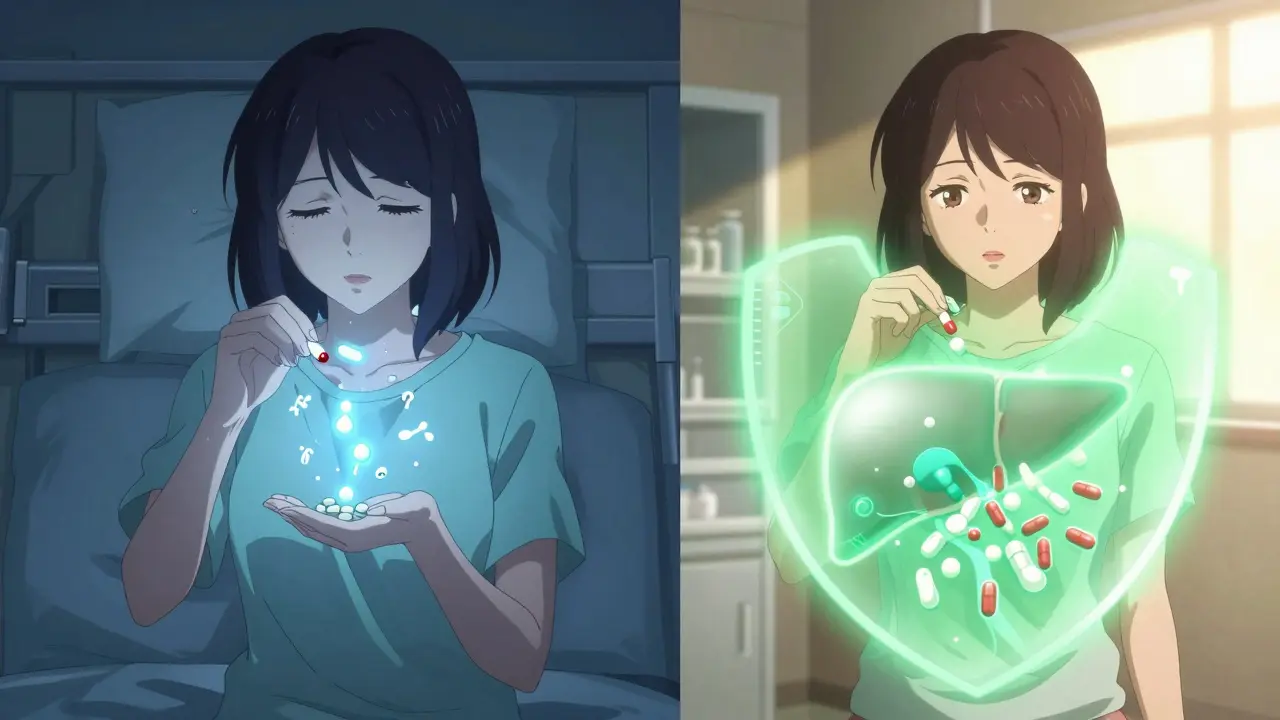
There are only two antibiotics-and one antifungal-that actually reduce how well birth control works: rifampin, rifabutin, and griseofulvin. Rifampin and rifabutin are used to treat tuberculosis and some serious bacterial infections. They work by turning on liver enzymes that break down hormones faster. This means your body clears out the estrogen and progestin in birth control pills before they can do their job. Studies show rifampin can drop estrogen levels by up to 50%. That’s enough to make birth control unreliable. Griseofulvin, an older antifungal used for nail or skin infections, has a similar effect. It’s rarely prescribed today, but if you’re taking it, you still need backup contraception. All other antibiotics? They don’t touch your birth control.Common Antibiotics That Are Safe
You can take these without worrying about your birth control failing:- Amoxicillin (for strep throat, ear infections)
- Azithromycin (Zithromax, for sinus infections)
- Doxycycline (for acne, Lyme disease)
- Metronidazole (Flagyl, for bacterial vaginosis)
- Ciprofloxacin (Cipro, for UTIs)
- Clarithromycin (Biaxin)
- Erythromycin
- Nitrofurantoin (for urinary tract infections)
- Amoxicillin-clavulanate (Augmentin)
What About Other Drugs?
Antibiotics aren’t the only thing that can interfere. Other medications can also reduce birth control effectiveness:- Lamotrigine (for epilepsy) at doses above 300 mg/day
- Topiramate (for seizures or migraines) at doses over 200 mg/day
- Effavirenz and nevirapine (HIV medications)
- St. John’s wort (herbal supplement for depression)-this one can drop estrogen levels by nearly 60%
What Should You Do?
Here’s the practical advice, based on the latest guidelines from the CDC and ACOG:- If you’re prescribed rifampin or rifabutin: Use a backup method like condoms for 28 days after finishing the course.
- If you’re prescribed griseofulvin: Use backup contraception for one month after treatment.
- If you’re prescribed any other antibiotic: You don’t need backup birth control. Your pill is still working.
Why Do So Many People Still Believe the Myth?
A 2022 survey by Planned Parenthood found that 62% of women thought antibiotics reduced birth control effectiveness. Even more surprising: 43% had used backup contraception during antibiotic treatment-even when they were taking amoxicillin or azithromycin. Why? Because pharmacists still tell them to. A 2022 study in the Journal of the American Pharmacists Association found that 35% of pharmacists still advise backup contraception for all antibiotics. Many are simply repeating what they were taught decades ago. Social media makes it worse. Reddit threads, Facebook groups, and Instagram posts are full of stories like, “I got pregnant while on antibiotics,” without mentioning they were taking rifampin. The fear spreads faster than the facts.What About Rifaximin?
Rifaximin (Xifaxan) is often confused with rifampin because of the similar name. It’s used for traveler’s diarrhea and IBS. But here’s the key difference: rifaximin doesn’t get absorbed into your bloodstream. It stays in your gut. That means it doesn’t affect liver enzymes. It doesn’t interfere with birth control. The FDA confirmed this in 2022. Don’t assume all “rif-” drugs are the same. Check the name. Ask your pharmacist.
What If You’re Still Worried?
It’s okay to feel anxious. Birth control failure is scary. If you want to use condoms anyway while on antibiotics, go ahead. It’s not harmful. But know this: it’s not necessary for most antibiotics. If you’ve had a pregnancy scare while on birth control and antibiotics, don’t panic. Most likely, it wasn’t the antibiotics. It was missing a pill, vomiting after taking it, or taking it at inconsistent times. Birth control pills work best when taken at the same time every day. That’s the real risk factor.What’s Changing?
In January 2023, the FDA updated the labeling for all hormonal contraceptives. The new labels now clearly state: “Rifampin, rifabutin, and griseofulvin may reduce effectiveness. Other antibiotics do not affect effectiveness.” That’s a big deal. It means the official medical record now reflects the science. But it hasn’t reached every pharmacy counter yet.Final Takeaway
The truth is simple: only three drugs-rifampin, rifabutin, and griseofulvin-interfere with birth control pills. Every other antibiotic you’ve ever been prescribed is safe to take with your pill. You don’t need to double up on protection unless your doctor specifically tells you you’re on one of those three. Stop worrying about amoxicillin. Stop stressing over doxycycline. Your birth control is still working. If you’re ever unsure, ask: “Is this a rifamycin or griseofulvin?” If the answer is no, you’re good. The myth is outdated. The science isn’t. Trust the data-not the rumor.Do all antibiotics make birth control less effective?
No. Only three medications-rifampin, rifabutin, and griseofulvin-have been proven to reduce the effectiveness of birth control pills. All other common antibiotics, including amoxicillin, azithromycin, doxycycline, and metronidazole, do not interfere with hormonal contraception.
I took amoxicillin while on birth control. Should I worry about pregnancy?
No. Amoxicillin does not affect how birth control pills work. The CDC and ACOG both confirm there’s no need for backup contraception when taking amoxicillin or similar penicillin-based antibiotics. Your birth control remains effective.
What if I’m taking rifampin for tuberculosis?
If you’re taking rifampin or rifabutin, you need to use a backup method of birth control, like condoms, for 28 days after finishing the course. These drugs speed up how your body breaks down hormones, making birth control pills less effective. The CDC recommends this precaution to prevent unintended pregnancy.
Can I trust what my pharmacist says about antibiotics and birth control?
Not always. A 2022 study found that 35% of pharmacists still advise backup contraception for all antibiotics, even though the science says only rifamycins and griseofulvin require it. Ask your pharmacist to check if the antibiotic is rifampin, rifabutin, or griseofulvin. If not, backup contraception isn’t needed.
Does St. John’s wort affect birth control like antibiotics do?
Yes, and more strongly. St. John’s wort, a popular herbal supplement for depression, can reduce estrogen levels by up to 57%. It works the same way as rifampin-by increasing liver enzymes that break down hormones. If you’re taking birth control, avoid St. John’s wort unless your doctor approves an alternative.
Why do some doctors still recommend backup contraception with antibiotics?
Some providers stick with the old advice out of caution or because they weren’t trained on the latest guidelines. The American Academy of Family Physicians has taken a conservative stance, suggesting backup contraception as a precaution. But major organizations like ACOG and the CDC agree: for non-rifamycin antibiotics, it’s unnecessary. The risk of pregnancy is extremely low without those specific drugs.
Is there any new research on this topic?
Yes. In 2023, the FDA updated birth control labels to clearly state which drugs interfere and which don’t. Current research is now focusing on whether obesity affects how these interactions work-women with a BMI over 30 already have a higher risk of contraceptive failure, and scientists are studying whether antibiotics might play a role in that group.


Comments
Shawn Peck January 30, 2026 AT 17:32
Look, I don’t care what the CDC says-I got pregnant on amoxicillin. My pill was fine, I took it every day, but boom-baby. So yeah, maybe the science says one thing, but real life doesn’t always follow the textbook. Don’t gamble with your future just because some study says it’s ‘safe.’
Niamh Trihy January 30, 2026 AT 22:54
Thanks for laying this out so clearly. I’ve been telling my patients this for years, but pharmacists still hand out those warning stickers like they’re candy. The real issue isn’t the science-it’s the inertia in healthcare systems. People are scared, and it’s easier to say ‘use condoms’ than to explain liver enzyme induction. But we owe it to women to give them accurate info, not fear-based assumptions.
Sarah Blevins February 1, 2026 AT 06:58
The data is clear, but the persistence of this myth reflects a deeper failure in medical communication. The FDA update in 2023 was a step forward, but without standardized training for pharmacists and physicians, labeling changes are performative. The 35% of pharmacists still giving outdated advice are not malicious-they’re misinformed. This is a systems problem, not a knowledge gap.
Jason Xin February 1, 2026 AT 09:46
Wow. So the entire medical establishment has been scaring women for 50 years over a drug that’s basically only used for TB now? And we still can’t get rid of the warning? I mean, I get it-liability, fear, laziness. But also… wow. Imagine if we applied this same logic to every other medication. ‘Oh, you’re taking ibuprofen? Better not drive. Just in case.’
Yanaton Whittaker February 1, 2026 AT 21:50
AMERICA IS BEING MANIPULATED BY PHARMA AND THE CDC! 🇺🇸 They want you to think it’s safe so you’ll keep taking the pill and not demand real healthcare! Rifampin? That’s just the tip of the iceberg. What about the 5G that messes with your hormones? 🤔💊
Kathleen Riley February 3, 2026 AT 21:43
One is compelled to interrogate the epistemological foundations upon which this myth has been perpetuated. The conflation of correlation with causation, the anthropomorphic attribution of agency to pharmaceutical agents, and the sociocultural reinforcement of medical paternalism collectively constitute a hegemonic narrative that subordinates empirical inquiry to institutional inertia. The persistence of this belief is less a function of ignorance than of structural power.
Beth Cooper February 4, 2026 AT 09:46
Okay but what if the real reason antibiotics mess with birth control is because Big Pharma doesn’t want you to know that your gut microbiome controls your entire hormonal system? They’re hiding the truth! The gut absorbs estrogen-everyone knows that! They just changed the science to sell more condoms. Also, I heard the moon affects progesterone. Coincidence? I think not. 🌕
Donna Fleetwood February 5, 2026 AT 12:50
Thank you for this. I’ve been terrified every time I’ve had to take antibiotics. I’ve used condoms for years even when I didn’t need to-and I’m so tired of the fear. This is the first time I’ve seen someone say it plainly: you’re not broken, your pill isn’t failing, and you’re not being reckless. It’s okay to breathe again.
Diana Dougan February 7, 2026 AT 10:25
LOL at all these people acting like they just discovered this. I’ve been telling my friends since 2018 that amoxicillin doesn’t do shit. Also, you spelled rifampin wrong in the post. And why are you still using blockquote tags? This is 2025. Get with the times. 🙄
Bobbi Van Riet February 7, 2026 AT 12:28
I’m a nurse, and I’ve had so many patients come in crying because they thought they were going to get pregnant after taking a simple antibiotic. The anxiety is real. And honestly? Even if the science says it’s safe, if someone feels better using a backup method, that’s valid too. It’s not about being right-it’s about reducing fear. But yes, please stop telling people they need condoms for azithromycin. That’s just causing unnecessary stress. I wish more pharmacists would read the actual guidelines instead of just repeating what they heard in pharmacy school 20 years ago.
Natasha Plebani February 9, 2026 AT 03:45
The ontological rupture between pharmacological mechanism and perceived risk reveals a profound dissonance in the contemporary medical subject. The pill, as a technological object, is rendered unstable not by chemical interference, but by the symbolic weight of collective dread. The myth of antibiotic-mediated contraceptive failure functions as a ritual of control-an inoculation against bodily autonomy. To dispel it is not merely to correct a clinical error, but to dismantle a patriarchal epistemology embedded in institutional pedagogy.
Eliana Botelho February 9, 2026 AT 14:10
Wait, so you’re saying I didn’t need to use condoms when I took cipro for my UTI last year? But my friend’s cousin’s neighbor’s daughter got pregnant on amoxicillin and now she’s got twins and a divorce and a new dog named Condom? I mean… I know the science says one thing, but what if the universe has its own rules? What if the bacteria in my gut were vibing with my estrogen and the antibiotics just… disrupted the harmony? I don’t know, man. I just feel like I need to be extra careful. You can’t be too safe, right?
Darren Gormley February 10, 2026 AT 22:36
So let me get this straight. Only 3 drugs interfere? 🤨 And yet, every pharmacist I’ve ever talked to says ‘use condoms’. That’s not incompetence-that’s corruption. The NHS is lying to us. And don’t even get me started on St. John’s Wort. That’s a herbal weapon disguised as a supplement. 🇬🇧 #PharmaCoverup
Mike Rose February 11, 2026 AT 17:09
bro i took azithromycin and i got pregnant. so the science is wrong. also i think the government is hiding the truth about birth control. like… why do they even make these pills if they don’t work? 🤷♂️
Sheila Garfield February 12, 2026 AT 09:31
Thank you for this. I’ve been telling my sister for years that she doesn’t need to panic every time she takes antibiotics. I’m glad someone finally wrote this out properly. I hope it reaches more people. We’ve all been carrying this unnecessary stress for too long.