Most people don’t think about antidotes until something goes wrong. But if you or someone you care about takes medications regularly, knowing what to do in an overdose can save a life. Antidotes aren’t magic pills-they’re precise medical tools designed to undo the damage of specific drug overdoses. And time matters. Every minute counts.
Acetaminophen Overdose: The Silent Killer
Acetaminophen (known as paracetamol in Australia) is in more than 600 over-the-counter and prescription products. It’s safe at normal doses, but taking just 10 to 15 grams at once-about 20 to 30 regular tablets-can cause serious liver damage. The scary part? You might feel fine for hours, even a full day. By the time nausea or pain shows up, the damage is already spreading.
The antidote is N-acetylcysteine, or NAC. It works by restoring glutathione, your liver’s natural defense against toxins. But NAC only works well if given within 8 hours of ingestion. After that, its effectiveness drops sharply. If you take too much, don’t wait for symptoms. Call emergency services or go to the hospital immediately.
Hospitals give NAC intravenously in a 21-hour drip: 150 mg/kg over the first hour, then slowly over the next 20. Oral NAC is an option too, but it’s harder to keep down if you’re vomiting. The full oral dose is 133 grams, split into multiple doses. Either way, starting treatment early means you’re far more likely to walk out of the hospital without long-term liver problems.
Opioid Overdose: Naloxone Can Bring Someone Back
Opioids-like oxycodone, heroin, fentanyl, or even high-dose prescription painkillers-slow breathing until it stops. That’s what kills. But there’s a fast, simple antidote: naloxone.
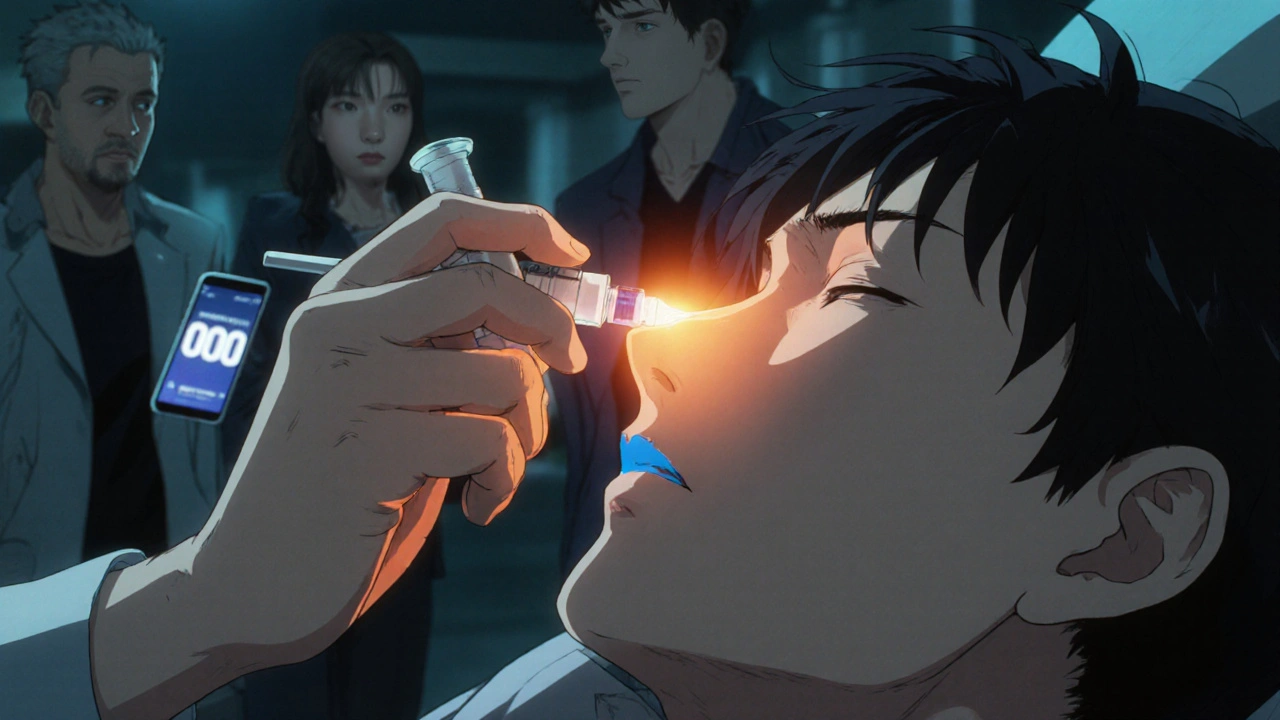
Naloxone blocks opioids from binding to brain receptors. It can reverse an overdose in under 2 minutes. It comes as a nasal spray (like Narcan) or an injection. In Australia, the Take-Home Naloxone Program has given out over 25,000 free kits since 2017. You can get one from pharmacies without a prescription.
Here’s how to use it: If someone is unresponsive, not breathing, or breathing very shallowly, give one spray into one nostril or inject into the thigh muscle. If they don’t wake up after 2 to 3 minutes, give a second dose. Then call triple zero (000). Naloxone wears off in 30 to 90 minutes. Opioids can last longer. That means someone can slip back into overdose after naloxone wears off. That’s why you must get them to emergency care-even if they seem fine after the first dose.
Some people wake up angry or panicked after naloxone. That’s because their body is suddenly deprived of the drug they’ve been relying on. It’s not personal-it’s biology. Keep them calm, stay with them, and wait for paramedics.
Benzodiazepine Overdose: When Calm Becomes Dangerous
Benzodiazepines like diazepam (Valium), lorazepam (Ativan), or alprazolam (Xanax) are prescribed for anxiety and sleep. But mixing them with alcohol or opioids increases overdose risk. Symptoms: extreme drowsiness, slurred speech, slow breathing, or passing out.
The antidote is flumazenil. It’s given as an IV drip, starting with 0.2 mg, then small increases every minute up to 3 mg total. But here’s the catch: flumazenil isn’t always safe. If someone has been taking benzodiazepines daily for months or years, using flumazenil can trigger sudden withdrawal-and that can cause seizures.
Most emergency teams avoid flumazenil unless it’s a clear, isolated overdose with no history of chronic use. Instead, they focus on supporting breathing with oxygen and monitoring heart rate. Sometimes, that’s all it takes. The body clears the drug on its own. The antidote is only used if breathing doesn’t improve and the patient is at risk of stopping altogether.
Toxic Alcohols: Methanol and Ethylene Glycol
These aren’t your typical medications-they’re found in antifreeze, windshield washer fluid, or some cleaning products. Accidental or intentional ingestion can be deadly. They don’t cause immediate vomiting or drowsiness. Instead, they turn into toxic acids in the body that attack the kidneys, brain, and eyes.
The antidote is fomepizole. It stops the body from turning the alcohol into poison. Dose: 15 mg/kg IV, then 10 mg/kg every 12 hours. It’s expensive-around $4,000 per treatment-but it’s safer and easier to manage than the old alternative: ethanol (vodka or whiskey). Yes, they used to give alcohol IV to block the poison. Now, fomepizole is preferred because it doesn’t make patients drunk or require constant blood sugar checks.
If fomepizole isn’t available, ethanol can be used as a backup. But it’s messy. You need to monitor blood alcohol levels, adjust doses constantly, and watch for low blood sugar. That’s why hospitals prefer fomepizole when they can get it. If you suspect someone swallowed antifreeze or cleaning fluid, call poison control immediately. Don’t wait for symptoms.
Methemoglobinemia: When Blood Can’t Carry Oxygen
This rare condition happens when certain drugs-like benzocaine (in some numbing sprays), dapsone, or nitrites-turn hemoglobin into methemoglobin. That version of hemoglobin can’t carry oxygen. Skin turns blue-gray. Breathing gets hard. The person may feel dizzy or confused.
The antidote is methylene blue. Given as an IV push over 5 minutes at 1-2 mg per kg of body weight. Don’t exceed 7 mg/kg total. It works fast. Within minutes, color returns to skin, and breathing improves.
But methylene blue isn’t safe for everyone. People with G6PD deficiency (a genetic condition) can have severe reactions. That’s why doctors check for it first. If you’re on a medication known to cause this and notice bluish skin or sudden shortness of breath, get help right away.
What You Can Do Now
You don’t need to be a doctor to help. Here’s what every household should know:
- Keep naloxone at home if anyone uses opioids, even as prescribed. It’s free in many community health centers in Australia.
- Store medications safely-out of reach of kids, in locked cabinets. Accidental overdoses in children are common.
- Know the signs of overdose: unresponsiveness, slow or stopped breathing, blue lips, pinpoint pupils.
- Call triple zero (000) immediately-even if you give naloxone or think it’s "not that bad." Emergency responders can do more than you can at home.
- Don’t wait for symptoms with acetaminophen. If you think you took too much, go to the hospital-even if you feel fine.

Myths That Can Kill
There’s a lot of misinformation out there. Don’t believe these:
- "Inducing vomiting helps." No. It can cause choking or aspiration. Don’t do it.
- "Drinking coffee or taking a cold shower wakes them up." False. These do nothing to reverse drug effects.
- "If they’re breathing, they’re fine." Not true. Breathing can slow to dangerous levels without being obvious.
- "Only drug users overdose." Most overdoses happen to people taking medications as prescribed-especially when mixed with alcohol or other drugs.
What to Expect at the Hospital
If you arrive with a suspected overdose, you’ll be assessed quickly. Staff will check your breathing, heart rate, and blood levels. They might do an ECG, blood tests, or a toxicology screen. They won’t just give you an antidote and send you home. Supportive care-oxygen, IV fluids, monitoring-is just as important.
For acetaminophen, they’ll plot your blood level on the Rumack-Matthew nomogram. That’s a chart that tells them if you need NAC. For opioids, they’ll watch you for at least 4 hours after naloxone to make sure you don’t relapse into overdose.
And if you’re being treated for a suicide attempt? You’ll be offered mental health support. Overdose isn’t always accidental. You’re not alone. Help is available.
Final Thoughts
Antidotes are powerful, but they’re not a substitute for prevention. The best antidote is knowing what you’re taking and how much. Keep a list of all your medications. Tell your doctor about everything-including supplements and alcohol. Never mix pills with alcohol. Store them safely. And if you’re worried about someone, don’t hesitate to act.
Overdoses happen faster than you think. But with the right knowledge, you can turn panic into action-and action into survival.
Can I keep naloxone at home in Australia?
Yes. Naloxone is available for free from community health centers, needle and syringe programs, and some pharmacies without a prescription. The Victorian Take-Home Naloxone Program has distributed over 25,000 kits since 2017. You can also buy it over the counter at pharmacies. It’s safe, easy to use, and can save a life.
How soon do I need to get help after taking too much acetaminophen?
Within 8 hours. After that, the antidote (NAC) becomes much less effective. Even if you feel fine, go to the hospital. Liver damage from acetaminophen doesn’t show symptoms until it’s advanced. By the time you feel sick, it may be too late for full recovery.
Is flumazenil safe for everyone with a benzodiazepine overdose?
No. Flumazenil can trigger seizures in people who take benzodiazepines regularly. Emergency teams usually avoid it unless it’s a clear, one-time overdose with no history of long-term use. Supportive care-like oxygen and breathing support-is often safer and preferred.
Can I use vodka instead of fomepizole for ethylene glycol poisoning?
In an emergency, yes-if fomepizole isn’t available. Ethanol (from vodka or whiskey) can block the toxin from forming. But it’s not ideal. It requires constant blood monitoring, causes intoxication, and can lead to low blood sugar. Fomepizole is safer, easier to use, and is the standard in hospitals.
What should I do if I find someone unresponsive and suspect an overdose?
Call triple zero (000) immediately. If they’re not breathing, start CPR. If you have naloxone and suspect opioids, give one dose in the nose or thigh. If they’re breathing but unconscious, place them in the recovery position-on their side with one leg bent. Don’t leave them alone. Wait for paramedics.


Comments
Sam Jepsen November 24, 2025 AT 13:51
This is the kind of info everyone needs to see. Seriously, keep naloxone in your glovebox or medicine cabinet if you have even one person in your life on opioids. It’s not just for "drug users"-it’s for grandmas, coworkers, teens with anxiety prescriptions. I’ve trained my whole family how to use the nasal spray. You don’t need to be a medic to save a life.
Yvonne Franklin November 24, 2025 AT 20:31
NAC for acetaminophen is time-sensitive. Don’t wait for nausea. If you took too many Tylenol, go to ER even if you feel fine. Liver damage doesn’t hurt until it’s too late.
Bartholemy Tuite November 25, 2025 AT 23:15
Man I remember back in the day when hospitals would just pump your stomach or give you vodka IV for antifreeze poisoning. Now we got this fancy fomepizole that doesn’t make you drunk or crash your blood sugar. Progress is wild. Still costs a fortune though. I work in an ER in Dublin and we’ve had to beg for it twice this year. Pharma companies really cash in on lifesaving stuff. But hey at least we got it now. Before it was either ethanol drip or pray. No joke.
Neoma Geoghegan November 26, 2025 AT 08:05
Flumazenil is a double-edged sword. Chronic benzo users? Don’t touch it. Seizures don’t play. Supportive care > quick fix. Oxygen. Monitoring. Patience. That’s the real hero here.
Natashia Luu November 27, 2025 AT 00:31
Why are we normalizing the idea that people should just carry antidotes like they’re candy? This is a society that refuses to regulate pharmaceutical pricing but expects citizens to become amateur toxicologists? The real antidote is systemic change. Not nasal sprays in every purse.
akhilesh jha November 28, 2025 AT 07:00
What if you don’t live near a hospital? What if you’re in rural India and your cousin takes too much paracetamol? NAC isn’t available in most villages. We rely on home remedies. Sometimes it works. Sometimes it doesn’t. This info is great but it’s useless if you can’t access it.
Jeff Hicken November 28, 2025 AT 15:29
So let me get this straight. You’re telling me I can just walk into a pharmacy and get a life-saving drug for free but I can’t get a $100 painkiller without a 3-page form? This system is broken. And don’t even get me started on how they charge $4000 for fomepizole. Greedy bastards.
Vineeta Puri November 29, 2025 AT 08:28
This is an excellent, well-researched guide. I’ve shared it with my community health group. We’re organizing free naloxone training sessions next month. If you’re in the US or Canada and want to attend, DM me. No one should die because they didn’t know how to act.
Victoria Stanley November 29, 2025 AT 16:14
Just had to say thank you for writing this. My sister overdosed on Xanax and alcohol last year. They didn’t give her flumazenil because of her history. She’s okay now but I still think about how close we came. This post could’ve saved us months of fear.
Andy Louis-Charles November 30, 2025 AT 16:04
💯 This needs to be a public service ad. I’m printing this out and handing it to my coworkers. Also, if you’re reading this and you’ve ever taken more than 4 acetaminophen pills in 24 hours… check your liver enzymes. Seriously. 🩺
Douglas cardoza December 2, 2025 AT 04:56
Just got my free naloxone kit from the pharmacy. Super easy. Like a spray you just point and press. No needles. No training needed. My grandma asked me what it was. I told her it’s for when someone stops breathing from pain meds. She said "Oh, like when your uncle took too many pills?" I said yeah. She said "Then we need two."
Adam Hainsfurther December 2, 2025 AT 23:29
One thing missing: what about pets? Dogs eat pills all the time. Acetaminophen is deadly for cats. Naloxone can be used in dogs for opioid overdoses. Vets have protocols. Call Pet Poison Helpline immediately if your animal ingests meds.
steven patiño palacio December 4, 2025 AT 10:28
My father was prescribed oxycodone after surgery. He didn’t know mixing it with wine could kill him. He did. We got to the hospital in time. Naloxone saved him. I didn’t know how to use it until the paramedic showed me. That’s why this post matters. Knowledge isn’t power-it’s survival.
Akash Chopda December 6, 2025 AT 09:03
They don’t want you to know this. NAC is cheap. Fomepizole is expensive. Why? Because the system profits from illness. The antidotes are real. The cover-up is too. Wake up. The pills are poison. The cure is hidden. Call your reps. Demand transparency. This isn’t medicine. It’s control.