Ever walked into a pharmacy to buy cold medicine, only to find the shelf empty and a pharmacist asking for your ID? You’re not alone. That’s not a glitch in the system-it’s the behind-the-counter (BTC) model in action. These aren’t regular over-the-counter (OTC) drugs you can grab off a shelf like ibuprofen or antacid tablets. They’re not prescription-only either. They live in a gray zone: accessible without a doctor’s note, but only after a pharmacist checks your ID, logs your purchase, and asks if you have any questions.
This system wasn’t created to annoy you. It was built to stop meth labs. In 2006, the U.S. government moved pseudoephedrine-once sold freely in every supermarket-to behind-the-counter shelves. Why? Because criminals were using it to cook illegal methamphetamine. The solution wasn’t to ban it entirely. It was to make sure every bottle sold came with a pharmacist watching over it.
What Exactly Counts as Behind-the-Counter?
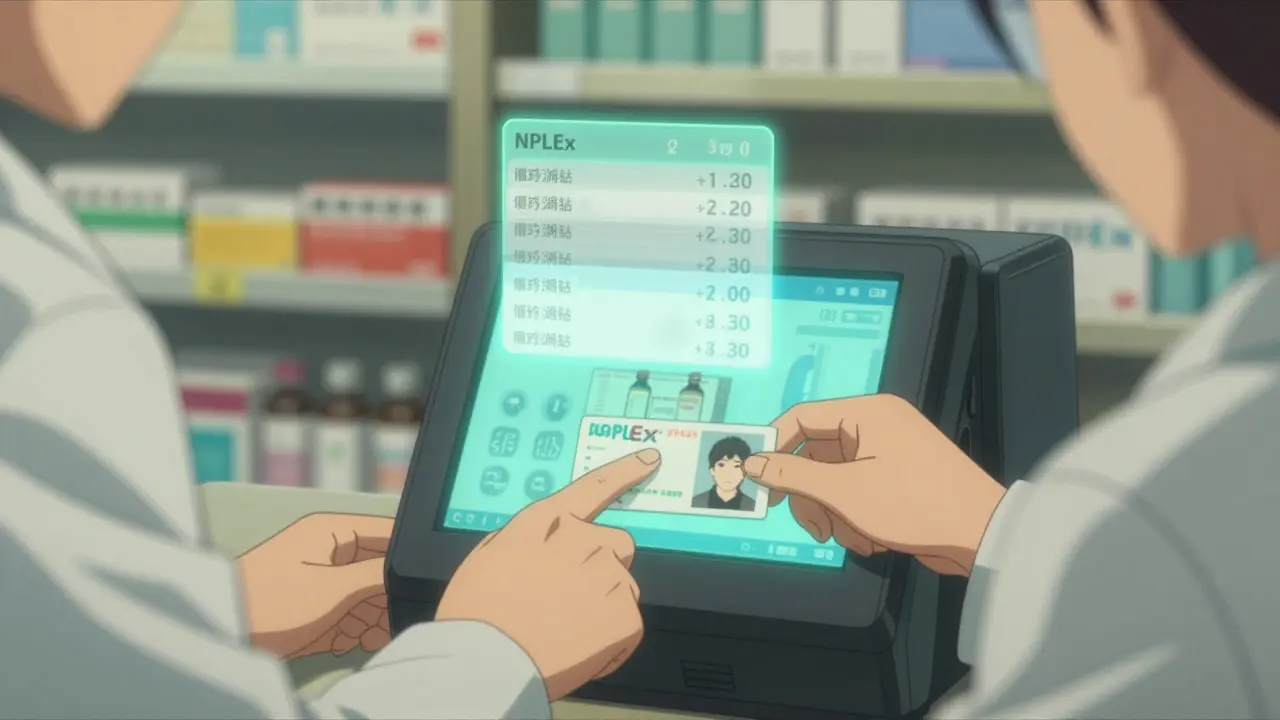
BTC medications fall between two worlds: prescription-only (POM) and general sales list (GSL) OTC drugs. You don’t need a prescription. But you can’t just walk in, grab the box, and head out. You must talk to a pharmacist. These drugs are stored behind the counter, often locked in a cabinet. You ask for them. The pharmacist asks you questions. They check your ID. They log your purchase in a national database called NPLEx. And then-only then-you get your medicine.
Here’s what you’ll commonly find behind the counter in 2025:
- Pseudoephedrine products (Sudafed, Claritin-D, Allegra-D): These are the most common. Each tablet usually has 30-60 mg of pseudoephedrine. Federal law limits you to 3.6 grams per day and 9 grams per 30 days. That’s about 6-12 tablets depending on strength. States like Oregon and Texas have their own caps, so what’s legal in one state might be restricted in another.
- Emergency contraception (Plan B One-Step, Next Choice): Available without a prescription to anyone 17 and older. You still need to show ID to prove your age. Before this rule, teens had to see a doctor or wait for a clinic. Now, you can get it at 2 a.m. after a night out. Studies show teen pregnancy rates dropped nearly half between 2007 and 2017 because of this change.
- Insulin (Walmart’s ReliOn brand): Regular insulin (Humulin R) and NPH insulin (Novolin N) are sold without a prescription at Walmart, Target, and other chains for $25-$40 per vial. This is a game-changer for people without insurance. Newer insulins like NovoLog still need a prescription, but these older versions are just as effective for many.
- Codeine cough syrups (in a few states): Oregon and Mississippi still allow low-dose codeine (up to 12.8 mg per dose) behind the counter. Most other states require a prescription now.
These aren’t random choices. Each one has a reason. Pseudoephedrine is powerful but dangerous if misused. Emergency contraception needs to be fast and private. Insulin is life-saving, and cost is a barrier for millions.
Why Not Just Make These OTC?
You might wonder: why not just put pseudoephedrine on the shelf like cough syrup? The answer is simple-effectiveness. Pseudoephedrine works better than phenylephrine, the OTC alternative found in most store-brand cold meds. Clinical studies show pseudoephedrine relieves nasal congestion in 72% of users. Phenylephrine? Only 38%. But because of its link to meth production, regulators didn’t want it freely available.
The BTC model solved that. People still get the better medicine. Pharmacies still track sales. Illicit labs? They moved on to other chemicals. But the system stayed.
Same with Plan B. If it were fully OTC, minors could buy it without anyone knowing. If it were prescription-only, many wouldn’t get it in time. BTC gives you access without bypassing age checks. It’s not perfect-but it’s the best compromise so far.
What Happens When You Buy a BTC Medication?
Here’s what you can expect when you ask for Sudafed or Plan B:
- You approach the counter and ask for the product by name.
- The pharmacist asks for a government-issued photo ID. Driver’s license, passport, or state ID. No exceptions.
- They scan your ID into a system called NPLEx. This tracks your purchases across all pharmacies in your state.
- They check your purchase history. If you’ve hit your monthly limit, you won’t get more.
- They ask you a few quick questions: “Are you taking any other meds?” “Do you have high blood pressure?” “Is this for you or someone else?”
- They hand you the product, often with a printed sheet of safety info.
This process takes 5-7 minutes. It’s not fast. But it’s designed to protect you and others.
Some people hate it. On Reddit, users complain about being turned away during cold season because they hit their limit. Others say pharmacists are rude or don’t explain anything. A 2022 study found that 18% of people seeking Plan B were delayed or refused-even though it’s legal. And a University of Michigan study found Black customers were over three times more likely to be questioned or denied than white customers, even when their buying patterns were identical. That’s not just inconvenient. It’s discriminatory.
Who Benefits From This System?
Pharmacists say they’re the unsung heroes of this system. They’re not just cashiers. They’re frontline health advisors. A Pharmacy Times survey showed 76% of customers felt more confident using BTC medications after talking to a pharmacist. That’s huge. For example, someone buying insulin for the first time might not know how to store it or what time of day to take it. A pharmacist can explain that in two minutes.
Patients with chronic conditions benefit too. People with diabetes who can’t afford $300 insulin vials now get ReliOn for $25. No prescription. No insurance. No red tape. Just access.
And then there’s the bigger picture. The FDA sees BTC as a bridge to make more prescription drugs available without a doctor’s visit. In 2023, they approved LoRez, a low-dose naltrexone for alcohol use disorder, as a BTC medication. That’s the first opioid-related treatment to get this status. Analysts predict five to seven more prescription drugs will move to BTC status by 2027-things like low-dose statins for cholesterol or mifepristone for gynecological conditions.
This isn’t just about cold medicine. It’s about rethinking how we deliver care. Pharmacists are trained to assess risk. They’re more accessible than doctors. And they’re already doing this job every day.

The Problems With BTC
But it’s not flawless.
State laws vary wildly. There are 28 different state rules for BTC drugs right now. One state might let you buy 9 grams of pseudoephedrine a month. Another caps it at 7.5. If you travel, you might get turned away because you’re “over limit” in a new state-even if you didn’t buy anything elsewhere. That’s confusing. And unfair.
Pharmacies pay a lot to comply. Each location spends about $1,200 a year on tracking software. Staff need 8 hours of training annually. That’s expensive for small pharmacies. Some rural stores just give up and stop carrying BTC meds altogether.
Access isn’t equal. Sixty million Americans live more than 10 miles from a pharmacy. If you’re in a rural town, you might have to drive 40 minutes just to buy Sudafed. That’s not access. That’s a barrier.
Documentation is poor. Many BTC product instructions are written at a college reading level. The American Medical Writers Association rated them just 3.2 out of 5 for clarity. Emergency contraception materials scored higher-4.1 out of 5-because they’re designed for urgency and simplicity.
What’s Next?
The future of BTC is growing. The market is expanding faster than regular OTC drugs-4.7% annual growth vs. 3.2%. By 2026, it could be worth $8.5 billion. That’s 7% of the entire OTC market.
More drugs will move to BTC status. But only if the rules get simpler. Right now, pharmacists have to juggle 28 different sets of state laws. That’s a nightmare. Experts like Dr. Joshua Sharfstein from Johns Hopkins warn that without federal standards, BTC will become a patchwork mess-where your access depends on where you live, not what you need.
For now, the system works well for most people. It gives you access to better medicine without a doctor’s appointment. It protects communities from drug abuse. It puts trained professionals between you and potentially risky substances.
But it’s not perfect. It’s clunky. It’s inconsistent. And sometimes, it feels like you’re being treated like a suspect just because you’re trying to buy medicine.
What’s needed isn’t more rules. It’s smarter rules. Uniform standards. Better training for pharmacists. And a system that doesn’t punish people for being sick-or poor-or Black.
Behind-the-counter isn’t going away. It’s here to stay. The question is: will we make it fairer-or just keep making it harder to use?


Comments
Andy Heinlein January 1, 2026 AT 08:21
Been buying Sudafed behind the counter for years and honestly it’s never been a big deal. Pharmacist asks two questions and I’m on my way. Better than some clerk not knowing what they’re selling.
Kristen Russell January 2, 2026 AT 06:29
Plan B being behind the counter saved me more than once. No shame in needing it fast. Pharmacist gave me the info I needed without judgment. That’s healthcare.
Dusty Weeks January 2, 2026 AT 08:33
why do we even need to show id for cold medicine?? 🤦♂️
Paul Ong January 3, 2026 AT 03:26
Y’all act like getting your ID scanned is a crime. If you want real medicine that works instead of sugar pills labeled as decongestants then deal with the 5 minute wait. Pseudoephedrine isn’t candy
Alex Warden January 3, 2026 AT 23:07
USA still letting people buy insulin without a prescription? That’s why we’re the best. Other countries make you beg for life saving drugs. Here you just walk in and get it. No bureaucracy
Matthew Hekmatniaz January 4, 2026 AT 16:19
I’m from a small town in Kansas. Our pharmacy stopped carrying BTC meds last year. Said the software cost too much. Now people drive 30 miles for Sudafed. That’s not access. That’s neglect.
sharad vyas January 5, 2026 AT 22:48
In India we get everything off the shelf. But I understand why here it’s different. Safety matters. Still, the system feels heavy when you’re just trying to treat a cold.
Sally Denham-Vaughan January 6, 2026 AT 16:57
My mom got denied Plan B last week because the pharmacist said she looked ‘too young’ even though she had ID. That’s not policy. That’s bias. And it’s wrong.
Richard Thomas January 7, 2026 AT 05:59
The BTC model is a fascinating compromise between autonomy and control. It acknowledges that some substances have dual utility - therapeutic and destructive - and attempts to navigate that tension without resorting to outright prohibition or reckless liberalization. The real failure isn’t the system itself, but the lack of standardization across states. Why should a person’s access to medicine depend on their ZIP code? That’s not public health. That’s administrative chaos. And the racial disparities in enforcement? That’s not just a flaw - it’s a moral failure. We’ve built a mechanism that works in theory but is corrupted in practice by human bias, underfunding, and fragmented governance. Fix the system, not the people trying to use it.
Bryan Anderson January 7, 2026 AT 06:56
I’ve worked in community pharmacy for 14 years. The BTC system lets us do our job. We’re not gatekeepers. We’re safety netters. I’ve prevented overdoses, caught drug interactions, and helped patients afford insulin. That’s why I support this model - even if it slows things down a bit.
Bill Medley January 9, 2026 AT 05:45
Uniform federal standards for behind-the-counter medications are not merely advisable - they are an imperative. Fragmented state regulations create inequity, inefficiency, and confusion. Harmonization would reduce compliance burdens, improve patient access, and ensure consistent clinical oversight. This is a policy opportunity that should not be squandered.
Lee M January 11, 2026 AT 04:19
You think this is about cold medicine? Nah. It’s about control. They don’t trust you with a bottle. They don’t trust you to make decisions. They don’t trust you to be responsible. So they make you prove you’re not a criminal every time you need help. That’s not healthcare. That’s suspicion as policy.