Diabetes: Medications, Metformin Alternatives & Practical Care
Most people with type 2 diabetes start with metformin, but that’s not the only route. If metformin causes side effects or doesn't control your blood sugar enough, there are several other meds and simple habits that help. This page summarizes the common drug choices, what they do, and clear day-to-day steps you can take to manage diabetes smarter.
Medications to know
Metformin lowers liver glucose production and helps insulin work better. It’s usually first-line because it’s effective and well-studied. If metformin doesn’t fit you, here are common alternatives:
- Alpha-glucosidase inhibitors (acarbose, miglitol): These slow carbohydrate digestion and blunt post-meal blood sugar spikes. Expect digestive side effects like gas and bloating, especially early on.
- DPP‑4 inhibitors (example: sitagliptin/Januvia): They boost the body’s own insulin response after meals with few side effects and low risk of low blood sugar.
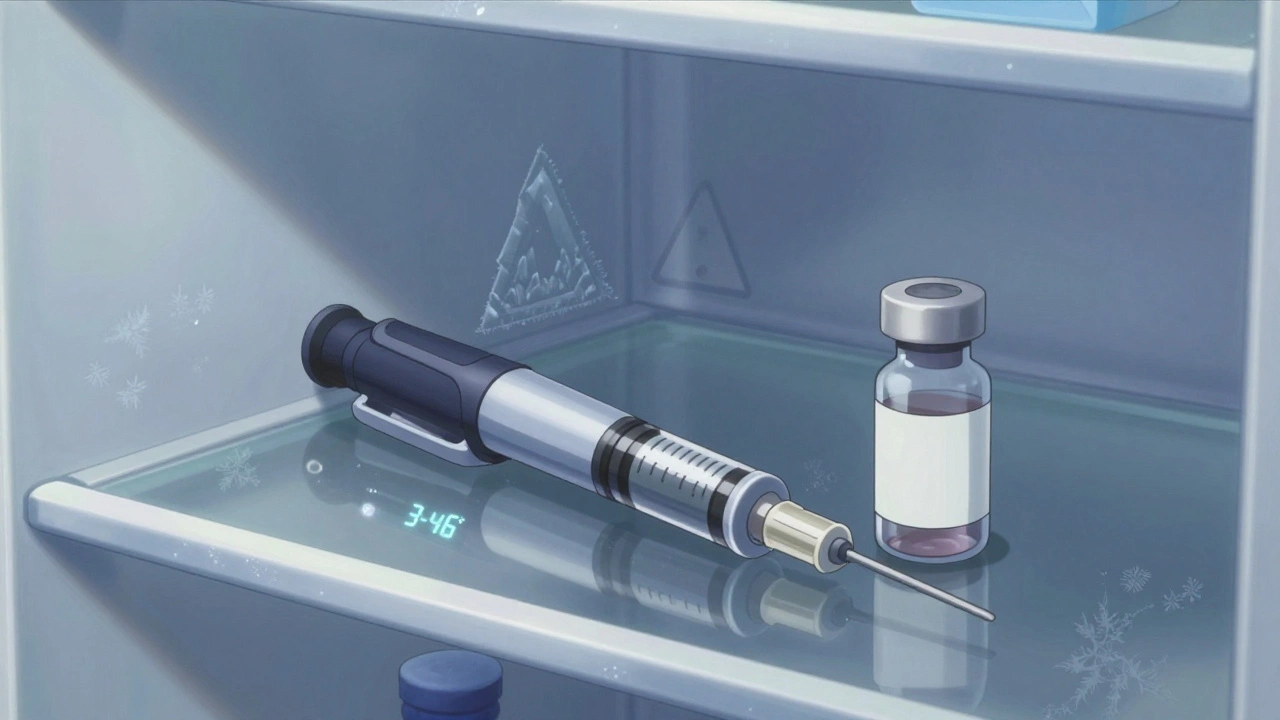
- GLP‑1 receptor agonists (example: liraglutide/Victoza): These reduce appetite, help weight loss, and lower blood sugar. They’re injected and can cause nausea at first.
- SGLT2 inhibitors (example: canagliflozin): They help the kidneys remove excess sugar in urine and can lower weight and blood pressure. Watch for urinary tract infections and dehydration.
- Sulfonylureas and insulin: These increase insulin levels and are powerful at lowering blood sugar but carry higher risk of hypoglycemia (low blood sugar).
Talk with your prescriber about how well each option suits your kidneys, heart, weight goals, and lifestyle. Some meds pair well with metformin; others replace it.
Practical tips for daily management
Medications work best with simple daily habits. Monitor your blood sugar as recommended and keep a short log of readings, meals, and activity. That helps you and your clinician spot patterns quickly.
Focus on portion control and consistent carbs at meals. Small swaps—like whole grains instead of refined carbs, or a serving of vegetables before the main course—can cut post-meal spikes. Aim for 20–30 minutes of moderate activity most days; even brisk walking lowers glucose.
Know the signs of low blood sugar: sweating, shakiness, sudden hunger, confusion. Keep a quick sugar source (juice, glucose tablets) nearby. If you notice side effects—digestive issues, repeated infections, or dizziness—call your provider. Medication often needs tweaking for kidney function, weight changes, or other meds you take.
Finally, schedule regular A1c checks and talk about heart and kidney health. Diabetes care is more than pills: it’s a plan you adjust over time. If you want comparisons between metformin and specific alternatives like acarbose or miglitol, check the linked articles on this page for straightforward breakdowns and real-world tips.