PPI Safety Checker for Clopidogrel
Is Your PPI Safe With Clopidogrel?
This tool checks CYP2C19 enzyme interactions between clopidogrel and your proton pump inhibitor. Based on clinical evidence, determine if you're at risk of reduced antiplatelet effects.
When you take clopidogrel after a heart attack or stent placement, your blood is thinner. That’s the whole point - to stop clots from forming and causing another event. But if you’re also taking a proton pump inhibitor (PPI) for heartburn or stomach ulcers, you might be weakening clopidogrel’s effect without even knowing it. This isn’t a theoretical concern. It’s a real, measurable drop in how well your blood platelets are inhibited - and it could mean the difference between staying safe and having another heart attack.
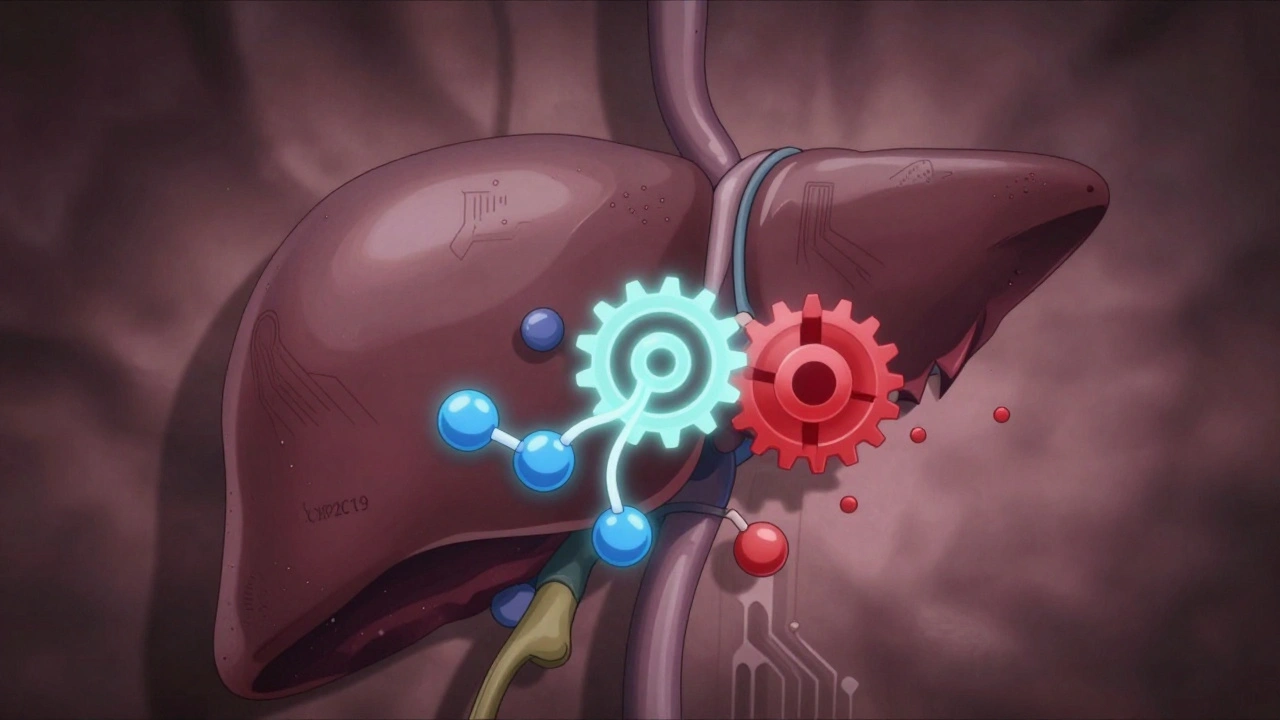
How Clopidogrel Actually Works
Clopidogrel doesn’t work right away. It’s a prodrug, meaning your body has to turn it into something active. That happens in your liver, using an enzyme called CYP2C19. Once activated, it sticks to platelets and blocks them from clumping together. Without this activation, clopidogrel is basically useless.
That’s where the problem starts. Many common PPIs - especially omeprazole and esomeprazole - also block CYP2C19. They’re designed to reduce stomach acid, but in doing so, they accidentally interfere with clopidogrel’s activation. Think of it like a factory line: clopidogrel is the raw material, CYP2C19 is the machine that turns it into the final product, and omeprazole is a wrench thrown into the gears.
Not All PPIs Are Created Equal
Here’s the key point most people miss: not every PPI does this. The strength of CYP2C19 inhibition varies dramatically between drugs.
- Omeprazole and esomeprazole are the strongest inhibitors. Studies show they can reduce clopidogrel’s active metabolite by up to 47%.
- Lansoprazole has a moderate effect - less than omeprazole, but still noticeable in some patients.
- Pantoprazole and rabeprazole barely touch CYP2C19. Their inhibition is so weak that multiple studies show no meaningful drop in antiplatelet activity.
One study tracked platelet reactivity in patients taking clopidogrel with omeprazole. The result? Platelet inhibition dropped from 84% to just 51%. In one patient, it vanished completely - even when doses were spaced 12 hours apart. That’s not a coincidence. That’s a direct, unavoidable interaction.
The Clinical Debate: Does This Actually Hurt Patients?
Here’s where things get messy. Yes, the pharmacology is clear. But does that translate to more heart attacks or strokes?
Some studies say yes. Dr. Deepak Bhatt’s 2009 research found a 50% higher risk of major heart events in patients taking clopidogrel with omeprazole. Other studies, like the COGENT trial, found no difference in outcomes - even though they confirmed the same pharmacodynamic drop in platelet inhibition.
Why the contradiction? One reason: real-world patients are complicated. Someone on clopidogrel and omeprazole might also be older, have diabetes, smoke, or take other meds. These factors can mask or amplify risks. Plus, many of the early studies were observational - not randomized trials.
But here’s what we do know for sure: if you’re a high-risk patient - say, you just had a stent placed - and your platelet inhibition drops below 30%, your risk of stent clotting goes up. That’s not speculation. That’s backed by platelet function testing data.

Who Should Avoid Omeprazole and Esomeprazole?
If you’re on clopidogrel, avoid omeprazole and esomeprazole - no exceptions. The FDA warned about this in 2009. The European Medicines Agency followed in 2010. The NHS Specialist Pharmacy Service says outright: "Other PPIs are considered safe with clopidogrel."
So what should you take instead?
- Pantoprazole - preferred choice. No significant interaction, widely available, and cheap.
- Rabeprazole - also safe. Short half-life, minimal CYP2C19 effect.
- Family history of ulcers? Taking NSAIDs? Over 75? Then you still need a PPI - but pick the right one.
According to a 2019 survey of 1,245 cardiologists, 72% chose pantoprazole over omeprazole when co-prescribing with clopidogrel. That’s not random. That’s experience.
Timing Doesn’t Fix It
You might think: "What if I take clopidogrel in the morning and the PPI at night?" That’s a common idea. But it doesn’t work.
The liver doesn’t care when you take the pills. CYP2C19 gets blocked for hours - sometimes days - by omeprazole. Even when doses are separated by 12 hours, the interaction still happens. The enzyme stays inhibited. The active metabolite still doesn’t form properly.
With pantoprazole or rabeprazole? Timing doesn’t matter. They don’t linger long enough to interfere.
What About Newer Drugs?
There’s good news on the horizon. Newer antiplatelet drugs like ticagrelor and prasugrel don’t rely on CYP2C19. They work directly. That’s why the European Society of Cardiology now recommends ticagrelor over clopidogrel for most heart attack patients.
And there’s a new class of acid reducers called potassium-competitive acid blockers (P-CABs). Vonoprazan is one. It blocks stomach acid just as well as PPIs - but doesn’t touch CYP2C19 at all. It’s in phase III trials and could replace PPIs entirely for clopidogrel users in the next few years.
What Should You Do Right Now?
If you’re taking clopidogrel and a PPI:
- Check which PPI you’re on. If it’s omeprazole or esomeprazole, talk to your doctor about switching.
- Don’t stop either drug on your own. Stopping clopidogrel increases clot risk. Stopping a PPI might cause bleeding.
- Ask if pantoprazole or rabeprazole is an option. They’re just as good for your stomach.
- If you’re unsure, ask for a platelet function test. It’s not routine, but it can show if clopidogrel is working.
And if you’re not on clopidogrel? Don’t worry. This interaction only matters if you’re using it for heart or stent-related reasons.
Why This Still Matters in 2025
Even though newer drugs are replacing clopidogrel, millions of people still take it. Many are older, have multiple conditions, and rely on it because it’s affordable and familiar. And many still get prescribed omeprazole out of habit - even though guidelines have changed.
Here’s a sobering stat: In 2010, over 21% of clopidogrel users in the U.S. were on omeprazole. By 2018, that dropped to 8.7%. That’s progress. But it means 1 in 12 people are still at risk.
Doctors aren’t ignoring this. Pharmacists are catching it. But patients? They often don’t know. Your pharmacist can check your med list. Your cardiologist can review it. But if you don’t ask, you might never find out.
The bottom line: clopidogrel and PPIs don’t always play nice. But you have control over which PPI you take. Don’t settle for the one your doctor prescribed by default. Ask: "Is this the safest option for my heart?"
Can I take omeprazole with clopidogrel if I space the doses apart?
No. Spacing doses - even by 12 hours - doesn’t prevent the interaction. Omeprazole inhibits the CYP2C19 enzyme for long periods, and the effect is cumulative. Studies show platelet inhibition still drops significantly, regardless of timing. Switch to pantoprazole or rabeprazole instead.
Is pantoprazole as effective as omeprazole for preventing stomach ulcers?
Yes. Pantoprazole reduces stomach acid just as effectively as omeprazole. Multiple studies show both drugs lower GI bleeding risk by about 70% in patients on dual antiplatelet therapy. The only difference is pantoprazole doesn’t interfere with clopidogrel’s effectiveness.
Should I stop taking clopidogrel if I need a PPI?
Never stop clopidogrel without talking to your doctor. Stopping it suddenly increases your risk of heart attack or stent clotting by up to 300%. Instead, switch your PPI to pantoprazole or rabeprazole. Those are safe with clopidogrel and still protect your stomach.
Are there any symptoms I should watch for if the interaction is happening?
There are no direct symptoms. The interaction reduces clopidogrel’s effect silently - you won’t feel it. That’s why it’s dangerous. The only way to know is through platelet function testing, which isn’t routine. If you’re on omeprazole and clopidogrel, assume the interaction is occurring and switch PPIs.
What if I’m on ticagrelor instead of clopidogrel?
Then you don’t need to worry. Ticagrelor and prasugrel don’t rely on CYP2C19 to work. You can safely take any PPI, including omeprazole, without reducing their antiplatelet effect. That’s one reason doctors now prefer them for most heart attack patients.

Comments
Lynn Steiner December 2, 2025 AT 23:39
OMG I JUST FOUND OUT I’M ON OMEPRAZOLE WITH CLOPIDOGREL 😭 I THOUGHT IT WAS FINE BECAUSE MY DOCTOR PRESCRIBED IT. I’M SWITCHING TO PANTOPRAZOLE TOMORROW. THIS POST SAVED MY LIFE. 🙏💔
Paul Keller December 4, 2025 AT 08:47
While I appreciate the clinical precision of this exposition, I must emphasize that the pharmacokinetic interference between CYP2C19 substrates and inhibitors is not merely theoretical-it is a well-documented, reproducible, and clinically significant phenomenon. The 47% reduction in active metabolite concentration observed with omeprazole is not an outlier; it is a consistent finding across multiple prospective cohorts. The disconnect between pharmacodynamic data and hard clinical outcomes in trials like COGENT likely stems from confounding variables, including patient compliance, comorbidities, and statistical power limitations. One must not confuse statistical non-significance with clinical irrelevance.
Elizabeth Grace December 5, 2025 AT 08:34
Ugh I hate when doctors just prescribe the first thing that comes to mind. My grandma’s on clopidogrel and omeprazole and she’s been fine… until she wasn’t. Got a stent clot last year. Now she’s on pantoprazole and feels like a new person. Why didn’t anyone tell us this before?? 😔
Joel Deang December 6, 2025 AT 13:26
so i was on omeprazole for like 3 yrs n just found out it might be ruining my clopidogrel?? 😳 i thought spacing em out worked?? like i take clopidogrel at 8am n omeprazole at 8pm?? turns out nope. lol. switched to pantoprazole yesterday. fingers crossed. 🤞 #medschoolfail
Roger Leiton December 7, 2025 AT 10:10
This is such an important post! 🙌 I work in pharmacy and see this ALL the time. Patients think ‘it’s just heartburn medicine’ and don’t realize it’s sabotaging their heart meds. I always check for clopidogrel + PPI combos and suggest pantoprazole or rabeprazole. The best part? They’re often cheaper too! 🤑 So many lives could be saved just by swapping a pill. Thanks for spelling it out so clearly!
dave nevogt December 9, 2025 AT 09:59
It’s fascinating how a biochemical interaction-so precise, so mechanistic-can be so easily overlooked in clinical practice. We treat the symptom, not the system. The liver doesn’t care about our intentions, our prescriptions, or our habits. It simply processes what’s given. And yet, we humans, with all our knowledge, still default to convenience over consequence. The fact that 1 in 12 people are still at risk isn’t just a statistical blip-it’s a failure of communication, of education, of systemic awareness. We have the science. We have the alternatives. What we lack is the collective will to change. And that’s the real tragedy.
Arun kumar December 10, 2025 AT 15:02
in india most doc just give omeprazole its cheap and availble. no one think about this interaction. i told my uncle to switch to pantoprazole after reading this. he was shocked. he said his doctor never told him. sad but true. 🤦♂️
Zed theMartian December 12, 2025 AT 10:52
Oh please. Another ‘medical authority’ telling us what to do. The FDA warned about this in 2009? And yet here we are, still talking about it like it’s news. The real issue? Pharma pushed omeprazole harder than clopidogrel. They made billions. Now they’re quietly pushing pantoprazole as the ‘safe’ alternative-same profit, different label. Don’t be fooled. The system is rigged. And you’re just another pawn in the pill game.
Ella van Rij December 13, 2025 AT 09:49
Wow. So after all this, the solution is… to take a different PPI? Groundbreaking. I’m sure my cardiologist will be thrilled to hear I’ve been ‘doing it wrong’ for 4 years because I didn’t read a Reddit post. 🙄 At least now I can blame the internet instead of my doctor. Thanks for the confidence boost, buddy.