Every year, over 36 million older adults in the U.S. fall - and nearly one in five of those falls leads to a serious injury like a hip fracture or brain bleed. Many of these falls aren’t just bad luck. They’re tied to medications that make people drowsy, dizzy, or unsteady. If you or someone you care for is taking a sedating drug - whether it’s for sleep, anxiety, pain, or muscle spasms - the risk of falling goes up. But here’s the good news: fall prevention isn’t just about grab bars and non-slip mats. It starts with the medicines on the shelf.
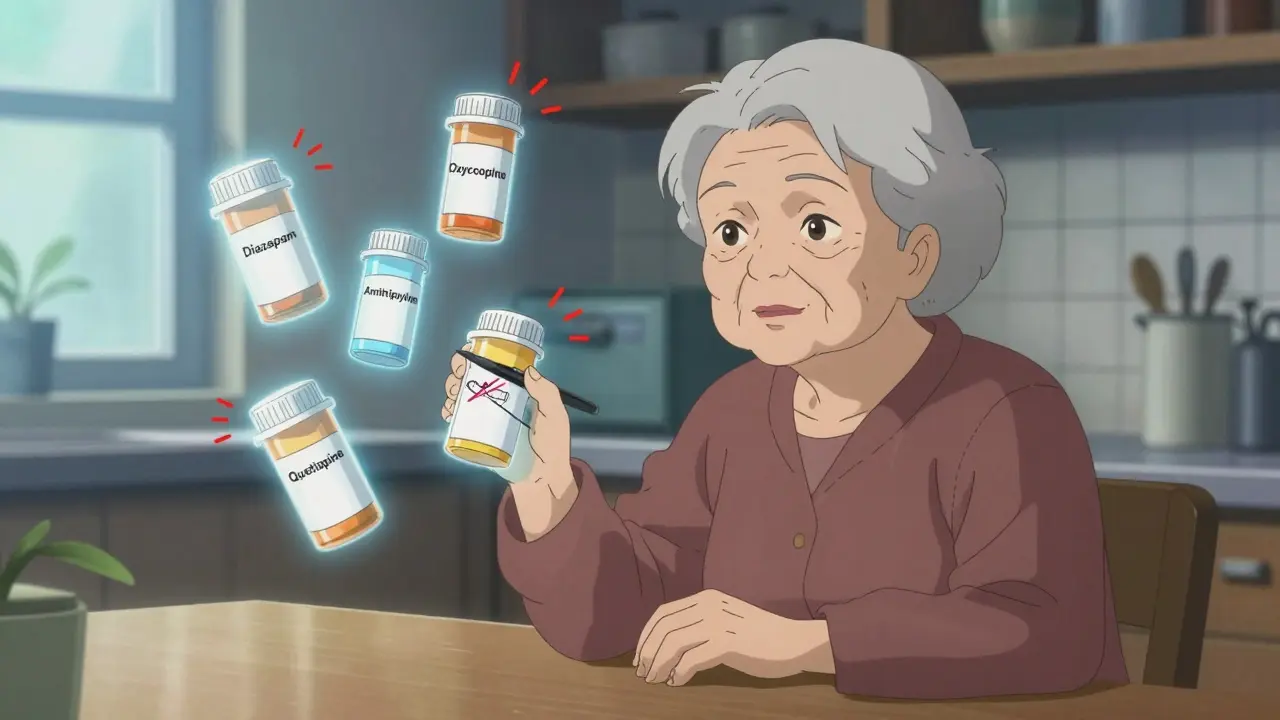
Which Medications Raise Fall Risk?
Not all sedating drugs are created equal, but many share the same dangerous side effects: slowed reaction time, blurred vision, low blood pressure when standing, and confusion. These are called Fall Risk Increasing Drugs, or FRIDs. Common ones include:- Benzodiazepines like diazepam (Valium) or lorazepam (Ativan) - often prescribed for anxiety or insomnia, but they linger in older bodies and cause dizziness.
- Antidepressants, especially tricyclics like amitriptyline - even at low doses, they can make you feel foggy and off-balance.
- Opioids like oxycodone or hydrocodone - pain relief comes with a heavy cost: drowsiness and poor coordination.
- Antipsychotics such as quetiapine or risperidone - sometimes used off-label for sleep or agitation in dementia, but they significantly increase fall risk.
- Muscle relaxants like baclofen - this one has the highest documented fall risk among its class.
- Antihypertensives - blood pressure meds that drop pressure too fast when standing up can cause sudden lightheadedness.
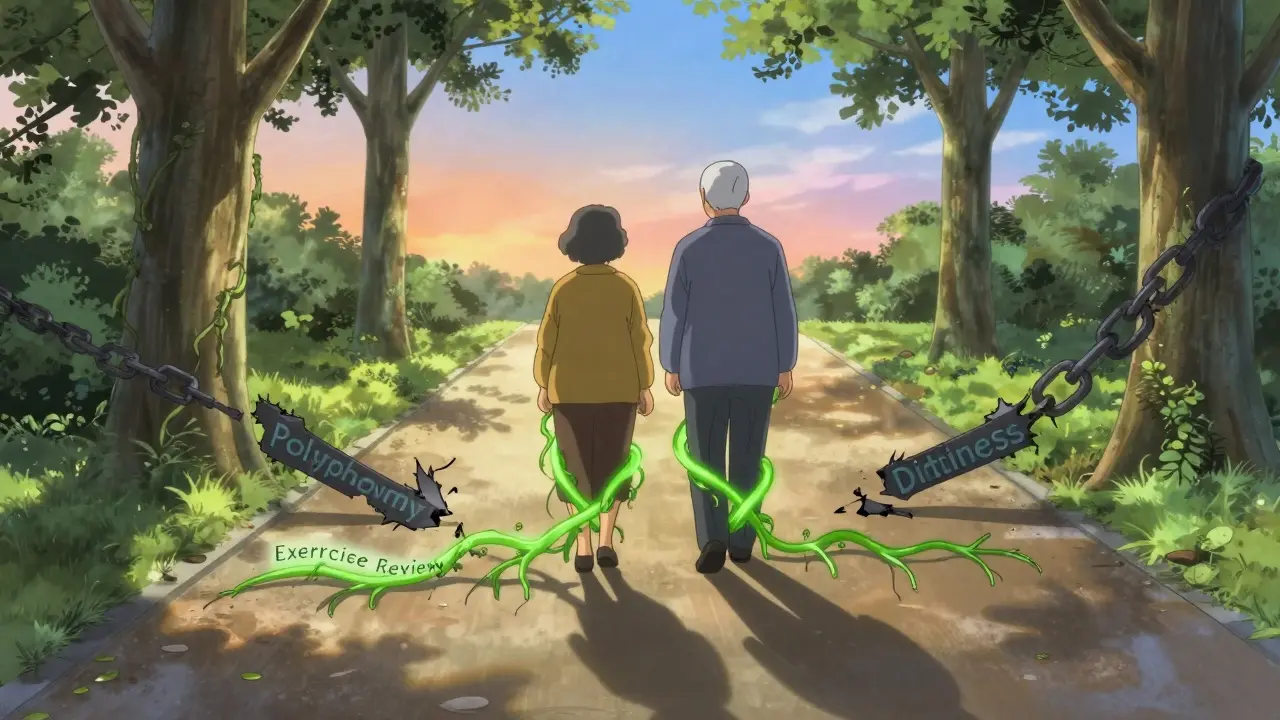
It’s not just one drug. The real danger is polypharmacy - taking three or more of these at once. Each extra pill stacks the risk. A 2021 study found that people taking five or more sedating medications were nearly four times more likely to fall than those taking none.
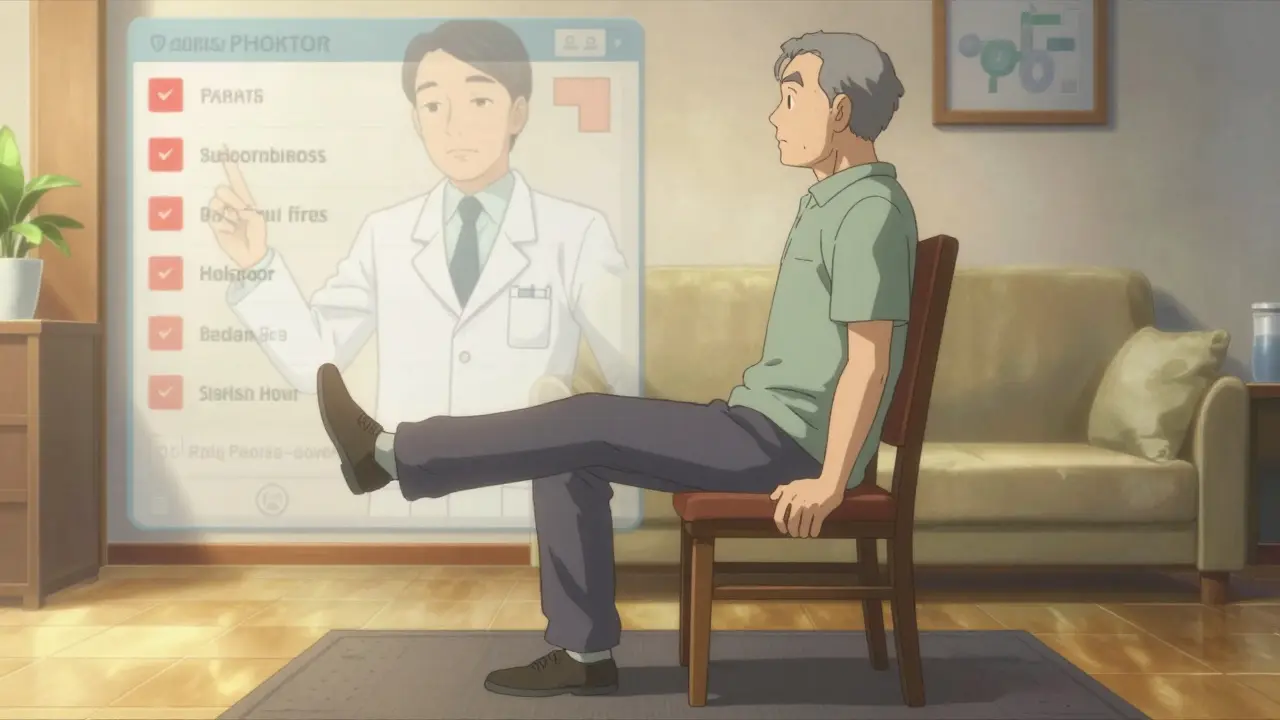
Medication Review: The Most Powerful Tool
The CDC’s STEADI-Rx program, developed in partnership with pharmacists and doctors, is now the gold standard for tackling this problem. It’s simple: screen, assess, intervene.Screening means asking: Have you fallen in the past year? Do you feel unsteady when standing or walking? If yes, it’s time for a full medication review. This isn’t just a doctor’s job - pharmacists are key players. They look at every pill, capsule, and patch on the list. They check for:
- Drugs on the Beers Criteria list of potentially inappropriate meds for older adults
- Drug interactions that make sedation worse
- Doses that are too high for aging bodies
- Drugs that haven’t been reviewed in over a year
What happens next? About 75% of the time, the recommendation is to switch to a safer alternative - not just stop everything. For example:
- Diazepam for sleep? Switch to cognitive behavioral therapy for insomnia (CBT-I), which works better long-term and has zero fall risk.
- Amitriptyline for nerve pain? Try duloxetine, which is less sedating and has proven benefits for pain without the dizziness.
- Quetiapine for nighttime agitation? Consider melatonin or light therapy instead.
One Reddit user, u/SeniorSafetyFirst, shared that after switching from diazepam to CBT-I, their nighttime falls dropped from 2-3 per month to zero in six months. That’s not luck - that’s smart prescribing.
Exercise Isn’t Optional - It’s Essential
Medication changes alone aren’t enough. The best results come when you combine drug review with movement. The Cochrane Review found that exercise programs reducing fall risk by 15-29% all had three things in common:- Balance training - standing on one foot, heel-to-toe walking
- Strength work - leg lifts, chair stands, resistance bands
- At least 12 weeks of consistent sessions - ideally 3 times a week, 30-90 minutes each
These programs don’t need fancy equipment. A simple chair-based routine done at home three times a week can cut fall-related fractures by 61%. And the benefits stick - people who keep moving stay steadier for years.
Many Medicare Advantage plans now cover fall prevention programs through physical therapy. Ask your doctor for a referral. If you’re not sure where to start, the National Institute on Aging offers free exercise videos online - no gym needed.
What About Vitamin D?
You’ve probably heard that vitamin D helps prevent falls. The truth? It’s complicated. The U.S. Preventive Services Task Force recommends 800 IU daily for older adults. But a major Cochrane review found no clear benefit when people already have normal levels. The key? Test first. If your blood level is below 30 ng/mL, then 1,000 IU daily can help. If it’s fine, extra pills won’t make you steadier.Why Is This So Hard to Do?
You’d think fixing this would be easy. But it’s not. Many older adults are afraid to stop their meds. They worry their anxiety, pain, or sleep problems will come back worse. Some doctors don’t feel confident in deprescribing. And pharmacists? Only 45% of them say they have enough time to do full medication reviews.There’s also a system problem. Most clinics don’t have alerts in their electronic records when someone is on five sedating drugs. No one gets flagged. No one gets called. The patient just keeps getting refills.
But change is happening. In 2023, the CDC expanded its STEADI toolkit with specific deprescribing guides for benzodiazepines. Over 1,200 pharmacists have now earned certification as Geriatric Pharmacotherapy Specialists. And Medicare now requires long-term care facilities to track fall risk - including medication use.
What You Can Do Right Now
If you’re caring for an older adult on sedating meds, here’s your action plan:- Make a complete list of every medication - including over-the-counter pills, patches, and supplements.
- Take it to the pharmacist. Ask: Are any of these linked to dizziness or falls?
- Ask the doctor: Can we try a lower dose? Is there a non-sedating alternative?
- Start a simple balance routine - even 10 minutes a day, holding onto a chair.
- Remove home hazards: loose rugs, poor lighting, cluttered hallways.
You don’t need to do everything at once. But if you tackle just one sedating drug and add one balance exercise, you’re already reducing risk. That’s more than most people do.
Final Thought: It’s Not About Taking Less - It’s About Taking Better
The goal isn’t to strip away all meds. It’s to make sure every pill still has a reason to be there. Older adults deserve to feel safe, steady, and in control. That starts with asking the right questions - about what’s in the medicine cabinet, and what’s missing from the daily routine.Can stopping a sedating medication cause withdrawal?
Yes, some sedating medications - especially benzodiazepines and certain antidepressants - can cause withdrawal symptoms like anxiety, insomnia, or tremors if stopped too quickly. That’s why tapering under medical supervision is critical. Never stop these drugs suddenly. Work with your pharmacist or doctor to create a slow, safe plan to reduce the dose over weeks or months.
How often should older adults have their medications reviewed?
At least once a year, but ideally every 6 months if they’re on multiple medications or have recently had a fall. Any time a new drug is added or an existing one is changed, a full review should happen. Many pharmacies now offer free medication therapy management (MTM) services - ask if you qualify.
Are over-the-counter sleep aids safe for older adults?
Most are not. Products like diphenhydramine (Benadryl) or doxylamine (Unisom) are anticholinergics - they cause drowsiness but also confusion, dry mouth, and urinary retention in older people. They’re linked to higher fall risk and even long-term cognitive decline. Safer alternatives include melatonin (at low doses), sleep hygiene changes, or CBT-I.
Can exercise help even if someone has already fallen?
Absolutely. In fact, people who’ve already fallen benefit the most from balance and strength training. Studies show that structured exercise reduces the chance of falling again by up to 43%. Programs designed for fall recovery focus on confidence-building, safe movement patterns, and core stability - all of which restore independence.
What should I do if my doctor refuses to change my medication?
Ask for a referral to a geriatrician or a pharmacist specializing in medication reviews. Many community pharmacies now offer free consultations with certified geriatric pharmacists. Bring your full med list and ask them to write a letter to your doctor outlining the risks and safer alternatives. You have the right to a second opinion - especially when your safety is at stake.
Next Steps: What to Do Today
- If you’re a caregiver: Schedule a pharmacist consultation. Bring the full med list - even the vitamins and herbal supplements. Ask: “Which of these could be making my loved one unsteady?” - If you’re an older adult: Start standing on one foot for 10 seconds each day, holding onto a chair. Do this three times a day. It’s the simplest way to build balance. - If you’re a healthcare provider: Use the CDC’s STEADI-Rx checklist during every visit with patients over 65. Flag any use of three or more FRIDs. Don’t wait for a fall to happen.Falls don’t have to be inevitable. With the right medication choices and a little daily movement, older adults can stay steady, independent, and safe - for years to come.

Comments
Glendon Cone January 1, 2026 AT 09:22
Big props to the author for laying this out so clearly 😊 I’ve seen too many older folks stuck on diazepam because ‘it’s always worked’ - but CBT-I? Game changer. My grandma switched last year and now she’s dancing in the kitchen again. No more midnight tumbles. Medication reviews should be mandatory at 65+.
Henry Ward January 2, 2026 AT 12:32
So let me get this straight - you’re saying we should just yank all the meds that keep seniors from screaming at 3 a.m. and call it a day? What about the people who actually need these drugs? This is just lazy medicine wrapped in feel-good buzzwords. You think balance exercises fix dementia-induced psychosis? Wake up.
Aayush Khandelwal January 3, 2026 AT 13:47
Respectfully, this is the kind of systemic intervention that’s been overdue in geriatric care. Polypharmacy isn’t just a ‘risk’ - it’s a pharmacological minefield. The Beers Criteria isn’t a suggestion, it’s a lifeline. And let’s not romanticize ‘exercise’ - it’s not yoga in the park, it’s neuroplasticity in motion. When you pair deprescribing with proprioceptive training, you’re not just preventing falls - you’re reclaiming autonomy. The real tragedy? Most clinics still treat meds like a checklist, not a living ecosystem.
Sandeep Mishra January 4, 2026 AT 01:28
I’ve worked with seniors for over 20 years - and I’ve seen the quiet ones who don’t say they’re dizzy, but they stop going out. They stop laughing. They stop living. This isn’t just about pills and balance beams. It’s about dignity. Tapering off a benzo isn’t just medical - it’s emotional. And yes, it’s scary. But when you walk someone through it - with patience, with a pharmacist holding their hand - they don’t just stop falling. They start trusting again. That’s the real win.
Kelly Gerrard January 4, 2026 AT 02:17
Vitamin D studies are inconclusive so dont waste money on supplements unless lab confirms deficiency. Exercise is non negotiable. Medication review essential. No exceptions. Period
Colin L January 5, 2026 AT 20:56
You know what’s worse than a fall? Being told your anxiety meds are ‘too sedating’ and then being handed a pamphlet on ‘sleep hygiene’ while your heart races and you can’t breathe. I’ve been on 4 of these ‘FRIDs’ for over a decade. My doctor says ‘try CBT’ like it’s a spa day. But when I tried to taper, I had tremors for three weeks and my therapist said I was ‘resistant.’ So now I’m just… stuck. And yeah, I fall sometimes. But I’m still here. And I’m still medicated. And no one has a clue what it’s like to be trapped between fear and fog.
Hayley Ash January 7, 2026 AT 18:27
Oh wow. So now we’re blaming the pills for falls? Next you’ll say gravity is a conspiracy. My uncle took nothing but aspirin and still faceplanted into his cereal bowl. Maybe it’s not the meds - maybe it’s that people are just old? Also, ‘duloxetine for nerve pain’? That’s a $200/month pill with its own list of side effects. This whole thing feels like a pharma ad disguised as public health advice. 🙄
kelly tracy January 8, 2026 AT 13:15
So let me get this straight - you’re telling me to stop my pain meds because I might trip? What if I can’t walk without them? And you think a 78-year-old with arthritis is gonna do ‘heel-to-toe walks’? That’s not prevention, that’s cruelty. And don’t even get me started on ‘CBT-I’ - like I have time to sit around talking about my sleep dreams instead of just taking a pill so I can rest. This isn’t empowerment. It’s guilt-tripping the vulnerable.