CHA₂DS₂-VASc Stroke Risk Calculator
Calculate Your Stroke Risk
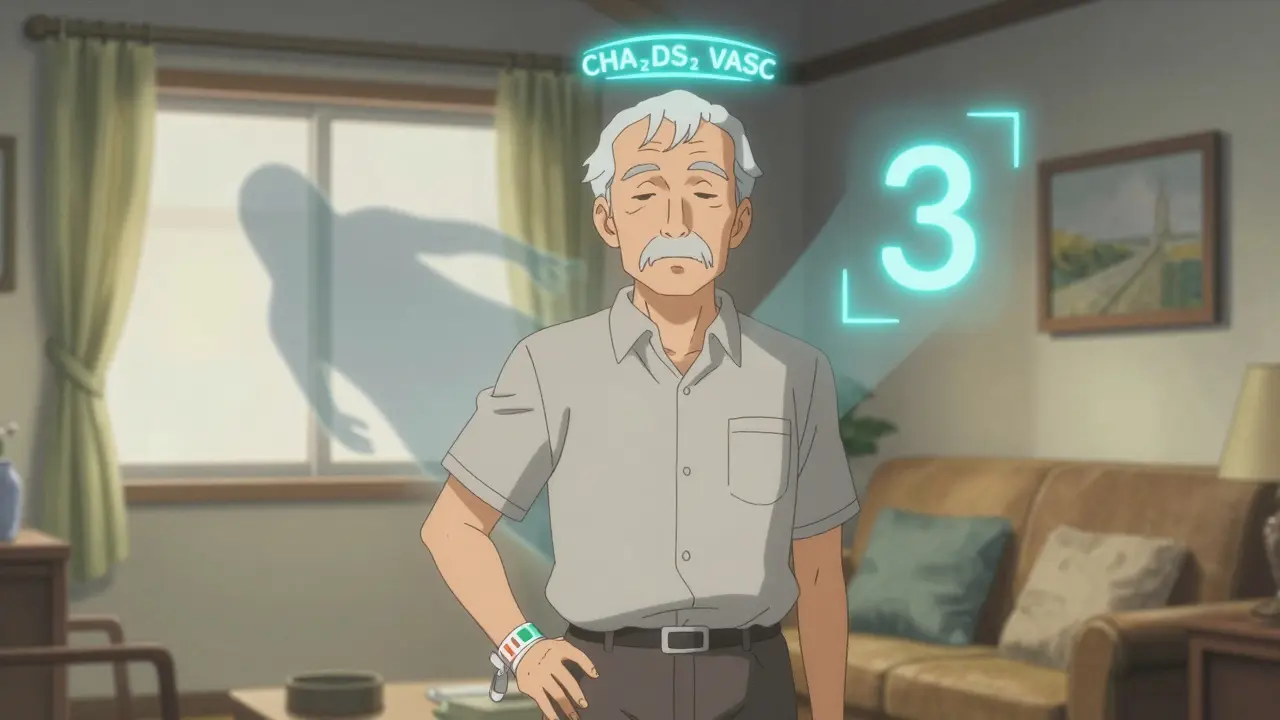
This tool calculates your CHA₂DS₂-VASc score to help determine your stroke risk if you have atrial fibrillation. The score helps doctors decide if you should take anticoagulants to prevent stroke.
Note: The CHA₂DS₂-VASc score is based on medical guidelines, but always discuss your treatment with your doctor. This tool does not replace medical advice.
Important: This calculator is for educational purposes only. Always discuss treatment options with your healthcare provider.
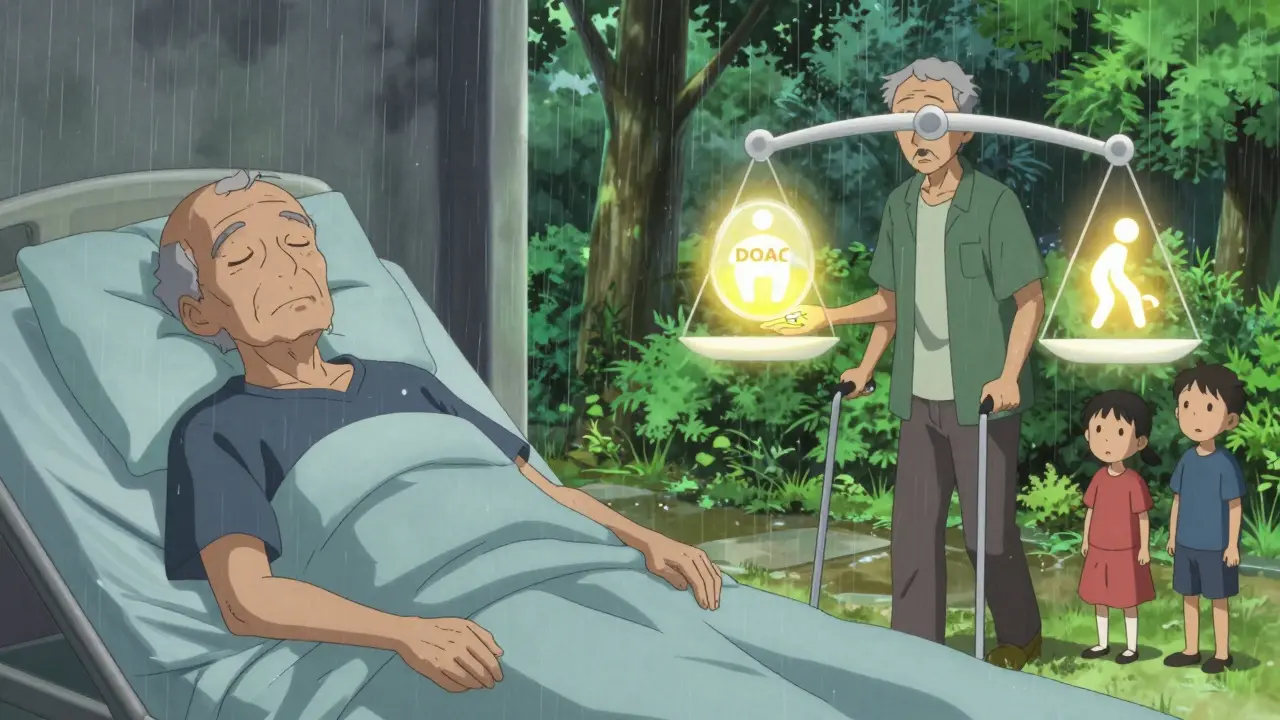
Many older adults on blood thinners are told to stop taking them because they’re at risk of falling. But here’s the truth: falling doesn’t mean you should stop anticoagulants. In fact, stopping them for fear of falls often puts you at greater risk of stroke - and death.
Consider this: a 78-year-old with atrial fibrillation has about a 3% chance of having a stroke each year if left untreated. That’s 3 in 100. Now, how many falls would it take for a blood thinner to cause a deadly brain bleed? About 295 falls in one year. Most people don’t fall that often. And yet, doctors still withhold these life-saving drugs because of a single fall or two.
Why Anticoagulants Are Still Safe - Even If You Fall
Anticoagulants like warfarin, apixaban, rivaroxaban, and dabigatran are prescribed to prevent strokes in people with atrial fibrillation and to treat blood clots in the legs or lungs. But as people age, falls become more common. About 30% of adults over 65 fall each year. In nursing homes, it’s more than half.
For decades, clinicians assumed that if a patient fell often, they shouldn’t take blood thinners. But research from the European Geriatric Medicine review (2023) and the American College of Physicians shows this thinking is outdated. The real danger isn’t the bleeding from a fall - it’s the stroke you could avoid.
The annual risk of a brain bleed from a fall while on a direct oral anticoagulant (DOAC) is between 0.2% and 0.5%. That’s less than one in 200. Meanwhile, the risk of stroke without anticoagulation in someone with a CHA₂DS₂-VASc score of 3 or higher is 1.5% to 3% per year - up to 15 times higher. The math doesn’t lie: preventing a stroke saves more lives than avoiding a rare bleed.
Don’t Use Fall Risk to Decide - Use the Right Tools
Doctors shouldn’t guess. They should measure. Two scores tell you what to do:
- CHA₂DS₂-VASc - measures stroke risk. If you’re a man with a score of 2 or higher, or a woman with 3 or higher, you need anticoagulation. Age, diabetes, heart failure, prior stroke - all count. Fall risk? Doesn’t matter.
- HAS-BLED - measures bleeding risk. A score of 3 or higher means you need closer monitoring, not no treatment. High blood pressure? History of bleeding? Too many meds? Fix those. Don’t stop the blood thinner.
Many patients are denied DOACs because they’ve had one fall. That’s not evidence-based. It’s fear. The Society of Hospital Medicine calls this practice - withholding anticoagulants just because of fall risk - a "Thing We Do for No Reason." It’s listed alongside other outdated habits that harm patients.
DOACs Are Safer Than Warfarin - Especially for Fallers
Not all blood thinners are the same. Warfarin has been around for decades, but it’s hard to manage. It needs frequent blood tests, interacts with food and other drugs, and increases the risk of brain bleeds. DOACs - apixaban, rivaroxaban, dabigatran, edoxaban - don’t need regular monitoring. They’re more predictable.
Studies show DOACs reduce the risk of brain bleeds by 30% to 50% compared to warfarin. That’s huge for someone who’s prone to falls. In fact, DOACs now make up 80% of new anticoagulant prescriptions in the U.S. because they’re safer and easier to use.
Some doctors try to lower the DOAC dose to "make it safer." Don’t. Taking less than the recommended dose doesn’t reduce bleeding - it just makes the drug less effective at preventing strokes. The European Geriatric Medicine review says this practice is dangerous and unsupported by data.
Stop Focusing on Falls - Start Fixing Them
The real solution isn’t stopping the blood thinner. It’s stopping the falls.
Here’s what works:
- Review all medications. Sedatives, sleep aids, blood pressure pills, and antidepressants can make you dizzy. Cut what you don’t need.
- Test your balance. The Timed Up and Go test takes less than a minute. Stand up from a chair, walk 3 meters, turn, walk back, sit down. If it takes more than 12 seconds, you’re at high fall risk. Physical therapy helps.
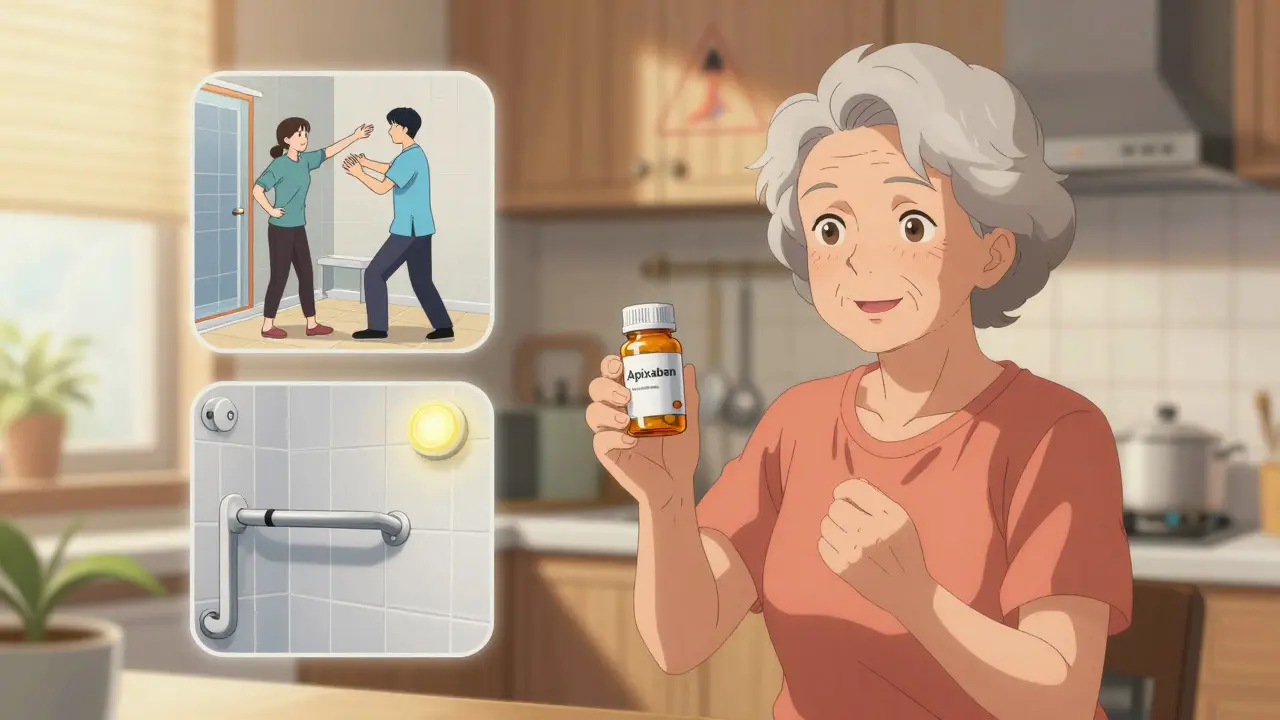
- Fix your home. Remove loose rugs. Install grab bars in the bathroom. Add nightlights. Clear clutter from hallways.
- Check your vision. Outdated glasses? Cataracts? Get them fixed. Poor vision is a top cause of falls.
- Treat low blood pressure. Standing up too fast can make you faint. If you feel lightheaded when you stand, tell your doctor. Simple changes can help.
A comprehensive fall assessment takes 30 to 60 minutes. It’s not quick. But it’s worth it. The American Medical Directors Association recommends this approach - not stopping anticoagulants. And it’s backed by decades of research.
When You Might Consider Stopping Anticoagulation
There are rare cases where stopping makes sense:
- You have active bleeding - like a stomach ulcer or recent brain bleed.
- You have uncontrolled high blood pressure (systolic over 180 mmHg).
- You have a known bleeding disorder - like severe hemophilia.
- You’re very frail, with a life expectancy under one year, and your stroke risk is low.
Even then, it’s not automatic. For someone with a CHA₂DS₂-VASc score of 5, the stroke risk is over 5% per year. Even if you’re 90 and frail, preventing one stroke could mean another year of independence. Shared decision-making matters. Talk to your doctor. Ask: "What’s my stroke risk? What’s my bleeding risk? What happens if I stop?"
What Happens When You Don’t Act
Too many people are left untreated. Studies show 20% to 30% of older adults with atrial fibrillation who should be on anticoagulants aren’t - mostly because of fall fears. This isn’t just a medical error. It’s a preventable cause of death.
One study found that patients who had a stroke while not on anticoagulants had a 40% higher chance of dying than those who were on them. And for every 1,000 people who avoid anticoagulants due to fall risk, about 20 will have a disabling stroke they could have avoided.
Medicare and other payers are now penalizing hospitals for under-treating atrial fibrillation. They’re pushing doctors to follow the guidelines. The message is clear: if you’re eligible, you should be on a blood thinner.
Real People, Real Choices
Mr. H, 78, had a CHA₂DS₂-VASc score of 3. He’d fallen twice in six months. He was scared. He chose not to take a blood thinner. Six months later, he had a stroke. He lost speech and mobility.
On the other hand, Mrs. L, 82, also fell often. But she and her doctor worked together. They cut her sleep meds. She got a physical therapist. They installed grab bars. She started apixaban. She’s still living independently. No strokes. No major bleeds.
The difference? One chose fear. The other chose action.
What You Can Do Today
If you’re on a blood thinner and worried about falls:
- Ask your doctor for your CHA₂DS₂-VASc and HAS-BLED scores.
- Request a fall risk assessment - don’t wait for them to offer it.
- Get your medications reviewed. Ask: "Which ones can I stop?"
- Have your vision checked. Update your glasses if needed.
- Check your home for hazards. A simple walk-through can save your life.
If you’re not on a blood thinner but have atrial fibrillation:
- Ask: "What’s my stroke risk?"
- Ask: "Is my fall risk enough to skip this?"
- Ask: "What are the alternatives?"
Don’t let fear make the decision for you. Use facts. Use tools. Use your voice.
Should I stop my blood thinner if I fall often?
No. Falling often does not mean you should stop anticoagulants. The risk of stroke from untreated atrial fibrillation is much higher than the risk of a serious bleed from a fall. Guidelines from the American College of Physicians and European Geriatric Medicine say fall risk alone is not a reason to stop blood thinners. Instead, focus on preventing falls through medication review, balance training, and home safety.
Are DOACs safer than warfarin for people who fall?
Yes. DOACs (like apixaban and rivaroxaban) are significantly safer than warfarin for people at risk of falls. They reduce the risk of brain bleeds by 30% to 50% and don’t require regular blood tests. They’re now the first choice for most patients with atrial fibrillation, even if they fall frequently. Lowering the DOAC dose is not recommended - it reduces stroke protection without lowering bleeding risk.
What’s the CHA₂DS₂-VASc score, and why does it matter?
The CHA₂DS₂-VASc score estimates your risk of stroke if you have atrial fibrillation. It counts factors like age, history of stroke, heart failure, diabetes, and high blood pressure. A score of 2 or higher in men (or 3 or higher in women) means you have moderate to high stroke risk and should be on anticoagulation - regardless of fall risk. This score guides treatment, not fear.
Can I still take blood thinners if I’m in a nursing home?
Yes. Over 50% of nursing home residents fall each year, but that doesn’t mean they should avoid anticoagulants. Studies show that residents with atrial fibrillation and high stroke risk benefit from DOACs, even in high-fall environments. The key is a comprehensive fall prevention plan - not withholding medication. Many nursing homes now use interdisciplinary teams to assess and reduce fall risk while keeping patients safely anticoagulated.
What are the only real reasons to stop anticoagulants?
You should only stop anticoagulants if you have active bleeding, uncontrolled high blood pressure (systolic over 180 mmHg), a known bleeding disorder, or if you’re very frail with a life expectancy under one year and your stroke risk is low. Fall risk alone is never a valid reason to stop. Stopping for any other reason increases your risk of stroke and death.
Staying safe on blood thinners isn’t about avoiding falls - it’s about managing them. The goal isn’t to live without risk. It’s to live with smart, evidence-based choices. Don’t let outdated fears keep you from the care you need.

Comments
Coral Bosley January 21, 2026 AT 18:45
They keep saying 'fall risk' like it's some magical excuse to let people die of strokes. I've seen grandmas fall three times a week and still walk into the kitchen to make tea. The real danger isn't the fall-it's the doctor who thinks they know better than the data.
Steve Hesketh January 23, 2026 AT 08:54
This is the kind of post that makes me believe medicine can still be human. So many elders are denied life because someone’s afraid of a lawsuit or a messy hospital chart. But the truth? It’s not about avoiding risk-it’s about choosing the right kind of risk. We don’t stop driving because we might get in a crash. We fix the roads, teach safer habits, and keep moving. Same here. Let’s stop treating older adults like fragile glass.
Philip Williams January 25, 2026 AT 05:04
The data presented here is not only statistically sound but clinically imperative. The CHA₂DS₂-VASc and HAS-BLED tools were developed precisely to remove subjective bias from anticoagulation decisions. The continued practice of withholding DOACs based on fall history reflects a systemic failure in geriatric education. Institutions must implement mandatory guideline-based decision support tools in EHRs to correct this preventable harm.
Barbara Mahone January 25, 2026 AT 09:29
I appreciate how this breaks down the numbers. My mom was taken off warfarin after one tumble in the bathroom. She ended up in the ER with a stroke six months later. No one ever mentioned DOACs. No one ever asked about her balance or meds. Just: 'Too risky.' It’s not risk. It’s neglect dressed up as caution.
MARILYN ONEILL January 25, 2026 AT 14:46
Wow. Just wow. I can't believe people still fall for this. What next? Should we give insulin to diabetics who trip over their own feet? This is just fear-mongering wrapped in fancy stats. People are dying from bleeding, not strokes. You think your math is smart? Try living with a brain bleed. It's not pretty.
Alex Carletti Gouvea January 27, 2026 AT 08:45
They want us to give blood thinners to every old person who can’t walk straight? This is why America’s healthcare is broken. We’re turning seniors into lab rats for some academic fantasy. If you can’t stand up without falling, maybe you shouldn’t be on a drug that could kill you in seconds.
Dee Monroe January 28, 2026 AT 20:20
There’s a quiet tragedy here that no one talks about: the way we’ve normalized abandoning older people when they become inconvenient. We don’t fix their homes. We don’t adjust their meds. We don’t teach them how to rise after a fall. We just pull the plug on the one thing that keeps them alive-because it’s easier than doing the hard work of caring. This isn’t medicine. It’s surrender. And it’s wrapped in a white coat.
Jerry Rodrigues January 29, 2026 AT 02:09
My dad was on apixaban after a stroke. He fell twice. We didn’t stop it. We got him a walker, removed the rugs, and put lights in every hallway. He’s 84 and still gardening. The fall risk isn’t the problem. The lack of action is.
Uju Megafu January 31, 2026 AT 00:53
Oh please. You think a few stats make you a hero? You’re just another doctor-worshipper ignoring the real cost. Bleeding doesn’t care about your scores. It doesn’t wait for your 'comprehensive assessment.' One fall. One head hit. And your grandpa’s gone. No second chances. No data to fix it. You’re gambling with lives and calling it science.
Jarrod Flesch January 31, 2026 AT 07:45
Big thanks for this. I’m a physio in Australia and I see this every week. Elderly patient on warfarin, falls, gets pulled off meds. We do a home safety check, fix meds, start balance training. Put them on apixaban. They go from wheelchair to walking the dog. It’s not magic. It’s just… common sense. 🙌
Stephen Rock January 31, 2026 AT 16:05
Look I get the stats but you’re talking about people who can’t even tie their shoes. You really think they’re gonna do all this home safety stuff? Nah. They’ll forget the grab bars. They’ll keep taking their sleep meds. And then boom. Brain bleed. And now you’re the one who killed them with your fancy guidelines. Stop pretending you’re helping. You’re just feeling good about yourself.
Glenda Marínez Granados January 31, 2026 AT 18:25
Oh so now we’re supposed to believe that a 90-year-old with three meds for dizziness and no vision should be on a blood thinner because ‘the math says so’? Cute. I’ve seen the aftermath. It’s not a math problem. It’s a moral one. And your math doesn’t fix the smell of blood on the linoleum.
Yuri Hyuga February 1, 2026 AT 08:55
This is precisely why I advocate for patient-centered geriatric care. The numbers don’t lie, but they don’t tell the whole story either. We must combine evidence with empathy. A CHA₂DS₂-VASc score isn’t just a number-it’s a person’s future. And that future deserves more than fear-based decisions. Let’s equip families, not just algorithms. 🌟
Sangeeta Isaac February 2, 2026 AT 08:17
my aunt got off warfarin after she tripped on the cat. six months later she had a stroke and forgot how to say ‘biscuit.’ we should’ve fixed the rug, not the meds. also why do doctors always act like they’re the first ones to think of this?
Ben McKibbin February 3, 2026 AT 19:37
Let me be blunt: if your doctor is stopping anticoagulants because of a fall, they’re either lazy, uninformed, or scared of liability. The guidelines are clear. The data is overwhelming. This isn’t a gray area. It’s a red flag. Demand your scores. Demand a fall assessment. Demand better. Your life isn’t a compromise.