Most people assume that if a generic drug has the same active ingredients as the brand name, it works the same way. That’s usually true-but not always. When it comes to generic combination drugs, small differences in inactive ingredients can make a real difference in how you feel, how well the medicine works, or even whether it causes side effects you didn’t have before.
What Exactly Is a Generic Combination Drug?
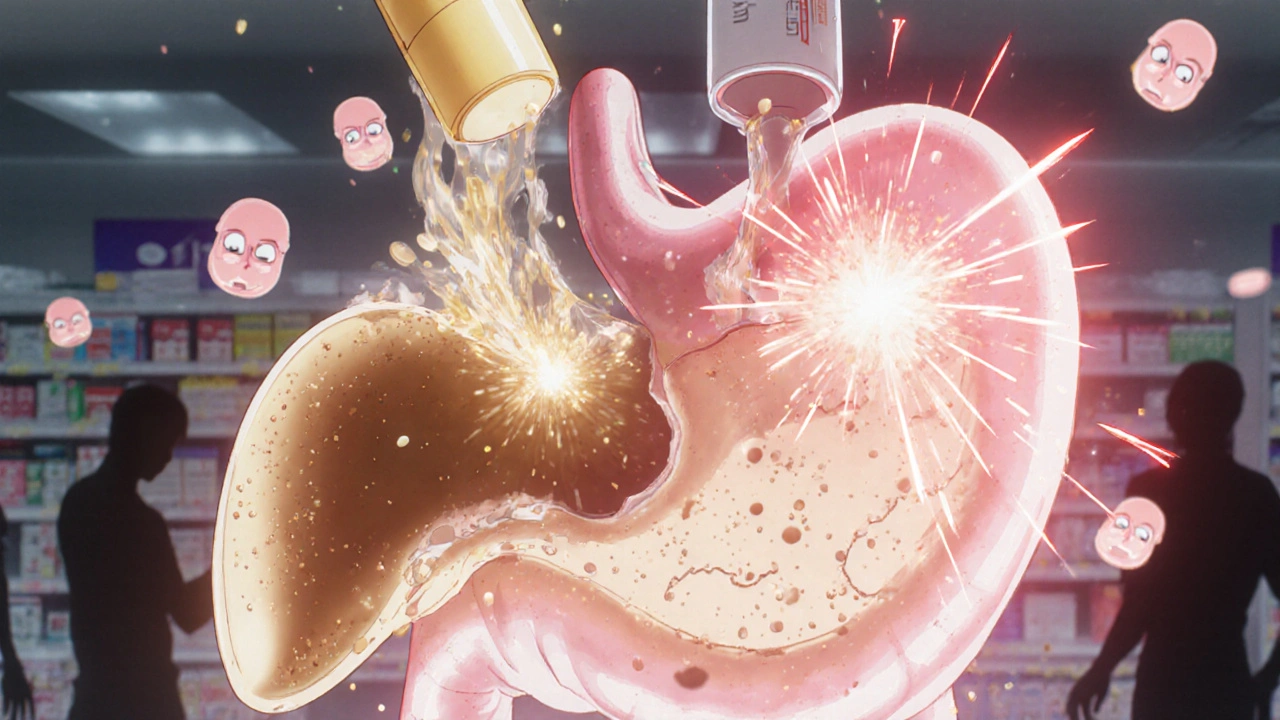
A combination drug combines two or more active ingredients into a single pill or inhaler. Think of Advair (fluticasone/salmeterol) for asthma, or Janumet (metformin/sitagliptin) for type 2 diabetes. These aren’t just two pills rolled into one-they’re carefully engineered to release each component at the right time and place in your body. Generic versions of these drugs must contain the exact same active ingredients, in the same strength, as the brand. That’s the law. But here’s the catch: the FDA allows generic makers to use different fillers, binders, coatings, dyes, and preservatives. These are called inactive ingredients. They don’t treat your condition, but they can change how the drug dissolves, how fast it’s absorbed, or even how your body reacts to it. In 2017, a study found that nearly half of all generic combination drugs had different inactive ingredients than their brand-name versions. That’s not a glitch-it’s allowed. But for some people, that difference matters.Why Do Inactive Ingredients Matter?
Imagine two identical engines-one in a luxury car, one in a budget model. Same horsepower, same parts. But the luxury engine uses premium fuel, better lubricants, and tighter tolerances. The budget one works fine for most drivers. But if you’re racing, or driving in extreme conditions, the difference shows up. That’s what happens with drugs. Inactive ingredients control how quickly the medicine releases into your bloodstream. For most people, it doesn’t matter. But for those on narrow therapeutic index (NTI) drugs, even a 5% change in absorption can mean the difference between control and crisis. NTI drugs include:- Levothyroxine (for thyroid disease)
- Warfarin (blood thinner)
- Phenytoin and other anti-seizure meds
- Cyclosporine (for transplant patients)
Real Stories: When the Generic Didn’t Work
People don’t always report these issues to their doctors. But online communities tell a clearer story. On Reddit’s r/pharmacy, users shared over 470 cases in 2022 where switching to a generic combination drug caused new side effects. One man switched from Janumet to a generic version and suddenly couldn’t eat without nausea. He’d never had that with the brand. His pharmacist checked the ingredients-same metformin, same sitagliptin. But the generic used a different binder. He switched back. The nausea vanished. Another woman with asthma switched from Advair Diskus to a generic inhaler. She started using her rescue inhaler 3-4 times a week instead of once a month. Her pulmonologist tested her lung function. Everything looked normal. But she felt worse. Her pharmacist looked up the device specs. The generic inhaler delivered 17% less drug to her lungs, according to independent lab tests. She went back to the brand-and her symptoms improved. A 2022 survey found that 34% of independent pharmacists had received patient complaints about generic combination drugs. The top issues? Gastrointestinal upset (41%), skin rashes (29%), and feeling like the medicine “just doesn’t work anymore” (22%).
The FDA’s Rules-And Their Gaps
The FDA says generics are bioequivalent if they deliver 80-125% of the brand’s drug into the bloodstream. That sounds precise. But here’s what that doesn’t catch:- How fast the drug releases over time
- Differences in how it’s absorbed in different parts of the gut
- How inactive ingredients interact with other meds you’re taking
- Device performance (like inhalers or injectables)
Who’s at Risk?
Not everyone needs to worry. But certain groups should be extra careful:- Elderly patients-slower metabolism, multiple meds, more sensitive to changes
- People with chronic conditions-like epilepsy, heart failure, or thyroid disease
- Patients on multiple drugs-inactive ingredients can interact with other meds
- Those with allergies-lactose, dyes, or preservatives in generics can trigger reactions
- People who’ve had bad reactions before-if a generic made you feel worse once, it likely will again
What You Can Do
You don’t have to avoid generics. But you do need to be smart about them. Ask your pharmacist:- Is this a generic combination drug?
- What’s the brand name it’s copying?
- Can you check the inactive ingredients? (They’re on the label.)
- Is this a narrow therapeutic index drug?

The Bigger Picture
Generics save the U.S. healthcare system billions. Medicare saved $1.67 trillion from 2006 to 2019 thanks to them. That’s huge. And for most people, generics are safe, effective, and life-changing. But medicine isn’t one-size-fits-all. A drug that works perfectly for your neighbor might not work for you-not because you’re different, but because the pill you got is different. The FDA knows this. In 2023, they started requiring more testing for complex combination products. The Generic Pharmaceutical Alliance promised to list all inactive ingredients on labels by 2025. And the NIH is spending $12.5 million to build better models predicting how formulation differences affect real patients. Until then, the power is in your hands. You don’t have to accept a generic if it makes you feel worse. You don’t have to pay more for the brand if you’re fine with the generic. But you do need to know the difference-and speak up when something feels off.What to Do If Your Generic Isn’t Working
1. Don’t stop taking it. Sudden withdrawal from some meds (like seizure or thyroid drugs) can be dangerous. 2. Write down your symptoms. When did they start? How bad are they? Did they get worse after switching? 3. Call your pharmacist. Ask them to check the manufacturer and lot number. Sometimes, different batches behave differently. 4. Ask your doctor for a prescription for the brand. Many insurers will approve it if you can show a documented reaction to the generic. 5. Report it. Use the FDA’s MedWatch system to report side effects from generics. These reports help the agency spot patterns and improve standards.Final Thought
Generic drugs are one of the best things to happen to modern medicine. They make life-saving treatments affordable. But they’re not magic. They’re chemistry. And chemistry, even when it’s “equivalent,” doesn’t always behave the same in every person. Your body isn’t a lab. It’s real. And if something feels wrong, it probably is. Trust yourself. Ask questions. Don’t let cost savings come at the price of your health.Are generic combination drugs always safe?
For most people, yes. Generic combination drugs work just as well as brand names for the vast majority of users. But for those on narrow therapeutic index drugs-like levothyroxine, warfarin, or anti-seizure medications-small differences in inactive ingredients can affect how the drug is absorbed. In rare cases, this leads to side effects or reduced effectiveness. Always monitor how you feel after switching.
How can I tell if my generic drug has different ingredients?
Look at the drug label. Inactive ingredients are listed in small print, usually under “Inactive Ingredients” or “Other Ingredients.” Compare this list to the brand-name version (you can find it on the manufacturer’s website or by asking your pharmacist). If you see different fillers, dyes, or preservatives, you’re seeing a formulation difference.
Can I request the brand-name version instead of the generic?
Yes. Your doctor can write “Dispense as Written” or “Do Not Substitute” on your prescription. Insurance may require prior authorization, especially for expensive drugs, but many will approve it if you’ve had a documented reaction to the generic. Authorized generics are another option-they’re made by the brand company but sold at lower prices.
Why do generic drugs cost so much less if they’re the same?
Brand-name companies spend billions on research, clinical trials, and marketing. Generic manufacturers don’t have to repeat those expensive studies. They only need to prove bioequivalence-which costs about $2 million. They also don’t spend on advertising. That’s why generics can be up to 85% cheaper. The savings come from skipping development costs, not cutting corners on safety.
What should I do if I think a generic is making me sick?
Don’t stop the medication abruptly. Contact your pharmacist and doctor right away. Keep a symptom journal: note when you switched, what symptoms started, and how severe they are. Ask your pharmacist to check the manufacturer and lot number. If symptoms improve when you switch back to the brand, that’s strong evidence. Report your experience to the FDA’s MedWatch system to help improve safety standards.

Comments
Tom Shepherd November 28, 2025 AT 05:42
I switched to a generic levothyroxine last year and started feeling like a zombie by noon. My doctor said it was 'all in my head' until I brought the label comparison. Turns out the generic had lactose and I didn't even know I was sensitive. Now I only take the authorized generic. Worth every extra dollar.
Rhiana Grob November 29, 2025 AT 17:17
This is such an important conversation that rarely gets had. The assumption that 'same ingredients = same effect' is dangerously oversimplified. I work in public health and see patients struggle with this all the time. The system needs better transparency-not just on labels, but in how insurers approve substitutions without patient input.
Frances Melendez December 1, 2025 AT 03:45
People who complain about generics are just lazy and want free brand-name drugs. If you can't handle a $5 savings, maybe you shouldn't be on medication at all. Stop being dramatic and take what the system gives you.
Jonah Thunderbolt December 2, 2025 AT 12:19
Let’s be real: the FDA’s '80–125% bioequivalence' standard is a joke. It’s like saying two sports cars are 'equivalent' if one goes 0–60 in 4.8 seconds and the other in 5.2 seconds-when you’re racing at 180 mph! The system is broken. And don’t even get me started on how they test dissolution in WATER?!?!? Our stomachs aren’t beakers!!!
Rebecca Price December 3, 2025 AT 02:49
As someone who’s been on multiple NTI drugs over the years, I can’t stress this enough: your experience matters more than any algorithm or regulatory threshold. If you feel different after a switch, document it. Bring the label. Ask for the authorized generic. You’re not being difficult-you’re being your own best advocate. And if your doctor dismisses you? Find a new one.
shawn monroe December 3, 2025 AT 11:06
As a pharmacist, I see this EVERY. SINGLE. DAY. The generic Advair inhalers? Total garbage. The actuator design is off by 15–20%. Patients think they're getting the same dose-but they're not. I now automatically flag combination drugs for NTI patients. I tell them: 'If you feel worse, come back. We'll swap it.' No judgment. Just science.
marie HUREL December 4, 2025 AT 21:49
I never thought about inactive ingredients until I got a rash after switching to a generic seizure med. Turns out it had a dye I’m allergic to. I didn’t even know dyes could be in pills. Now I always check the label. It’s not hard-just scroll down past the big print. Small thing, huge difference.
Lauren Zableckis December 6, 2025 AT 17:15
My mom switched to a generic Janumet and started having stomach cramps so bad she couldn’t work. She went back to the brand and it vanished. The pharmacist said 'it’s the same.' But it’s not the same if your body says so. I wish more people knew this.
Asha Jijen December 7, 2025 AT 14:47
generic is cheap and works for most people why make a big deal lol
Edward Batchelder December 9, 2025 AT 05:24
To Asha: I get it-cost matters. But imagine if your insulin, your blood thinner, or your seizure med stopped working because of a filler you didn’t know about. This isn’t about being expensive. It’s about safety. And for the 1 in 4 people who react? It’s life-changing. Let’s not dismiss real suffering because it’s inconvenient to fix.