When you have an autoimmune disease like rheumatoid arthritis, lupus, or Sjögren’s syndrome, it’s not just the pain that wears you down-it’s the functional impairment. Getting dressed, cooking a meal, holding a cup, or even walking to the mailbox can become exhausting, impossible tasks. This isn’t laziness. It’s your immune system attacking your body, combined with medication side effects, chronic inflammation, and the slow creep of deconditioning. The good news? Rehab and occupational therapy aren’t just helpful-they’re essential for keeping your life yours.
Why Functional Impairment Happens in Autoimmune Diseases
Functional impairment doesn’t come out of nowhere. It’s the result of three things working together: inflammation damaging your joints and muscles, medications causing fatigue or muscle weakness, and your body slowly losing strength because you’ve been avoiding movement to protect yourself. Over time, this creates a cycle: you hurt, so you rest, so you lose strength, so you hurt more. Studies show that up to 8% of people with autoimmune conditions experience moderate to severe functional decline within the first year. Women are three times more likely to be affected. The Health Assessment Questionnaire Disability Index (HAQ-DI) measures this decline. A score above 1.5 means you’re struggling with daily tasks. A score over 2? You’re likely unable to work or manage basic self-care without help.What Physical Therapy Actually Does
Physical therapy (PT) focuses on movement. It’s not about pushing through pain-it’s about moving smartly. During a flare, when your joints are swollen and hot, PT uses gentle isometric exercises-muscle contractions without joint movement-at just 20-30% of your max strength. This keeps your muscles active without worsening inflammation. As symptoms ease, therapists gradually increase intensity. Aerobic training kicks in at 40-60% of your heart rate reserve. That’s not running marathons. It’s walking on a treadmill at a pace where you can still talk, but not sing. Hydrotherapy-exercising in warm water (92-96°F)-reduces pain by 22% more than land-based workouts. The water supports your weight, reduces joint pressure, and soothes inflamed tissues. A 2022 study in the Journal of Autoimmunity found that people who started PT within 12 months of symptoms improved their HAQ-DI scores by 35-42%. That’s the difference between needing help to shower and doing it alone.Occupational Therapy: Reclaiming Daily Life
While PT helps you move, occupational therapy (OT) helps you do the things you need to do every day. OT doesn’t just teach you how to use a cane. It teaches you how to cook without your hands giving out, how to button a shirt when your fingers are stiff, how to sit at your desk without your wrists screaming. The 4 Ps rule is the backbone of OT: Prioritize what matters, Plan your day around energy levels, Pace yourself with frequent breaks, and Position your body to reduce strain. For example, instead of standing at the sink for 30 minutes washing dishes, you do 15 minutes, then rest 10. You use a dish rack to avoid bending. You switch to a lightweight mug with a wide grip. The Canadian Occupational Performance Measure (COPM) is the gold standard tool therapists use. A 2-point increase on its 10-point scale is considered clinically meaningful. That means if you went from struggling to hold a toothbrush to doing it without pain, that’s a win.PT vs OT: What Each One Covers
| Focus Area | Physical Therapy | Occupational Therapy |
|---|---|---|
| Primary Goal | Improve strength, mobility, endurance | Enable independence in daily tasks |
| Lower Body Function | 28% more effective (Timed Up and Go test) | Less focused |
| Upper Body Function | Modest improvement | 33% more effective (Arthritis Hand Function Test) |
| Activities of Daily Living | Indirect support | Direct intervention (dressing, eating, hygiene) |
| Key Tools | Underwater treadmills, goniometers, TENS units | Adaptive utensils, joint protection splints, voice-activated tech |

When Therapy Works Best-and When It Doesn’t
Rehabilitation shines during stable phases. When your Disease Activity Score (DAS28) is below 5.1, you’re likely to see real gains. But during a flare-when joints are swollen, fever spikes, or you’re on high-dose steroids-therapy needs to pause or shift dramatically. Pushing through pain during a flare doesn’t build strength. It triggers crashes. One major problem? Many therapists don’t understand central fatigue-the deep, brain-driven exhaustion that hits people with lupus or fibromyalgia. Dr. Alan Peterson’s 2021 JAMA commentary warned that 19% of rehab programs ignore this, leading to worse symptoms. If your therapist says, “Just push harder,” they’re not trained for autoimmune conditions. Also, not all rehab centers are created equal. Hydrotherapy helps-but 68% of rural clinics don’t have pools. TENS units, specialized equipment, and trained staff? Still rare outside major cities.What Patients Really Say
Reddit threads from r/ChronicIllness tell a clear story. 68% of users say aquatic therapy changed their lives. One person wrote: “After six months of graded exercise, my HAQ-DI dropped from 2.1 to 0.8. I went from being homebound to working part-time.” But 47% of negative reviews on Healthgrades complain about therapists ignoring flares. “They told me to ‘tough it out.’ I ended up bedridden for three weeks.” That’s not rehab. That’s harm. Success stories often involve adaptive tools: voice-controlled lights, smart thermostats, one-handed can openers. One woman with scleroderma said her voice-activated home system gave her back 31% of her independence. “I used to need help turning on the TV. Now I just say, ‘Alexa, turn on the news.’”The 70% Rule: How to Avoid the Boom-Bust Cycle
The biggest trap? The boom-bust cycle. You have a good day. You feel almost normal. You clean the house, run errands, go out with friends. Then you crash for days. It’s exhausting-and it sets you back. The solution? The 70% rule. Never push yourself beyond 70% of what you think you can do. If you feel you can lift 10 pounds, lift 7. If you think you can walk for 30 minutes, walk for 20. Track your energy using an activity diary or a wearable heart rate monitor. Your body’s warning signs are subtle: increased fatigue, brain fog, slight joint warmth. Learn them. It takes 8 to 12 weeks to master pacing. But once you do, your crashes shrink from 3.2 days to less than one.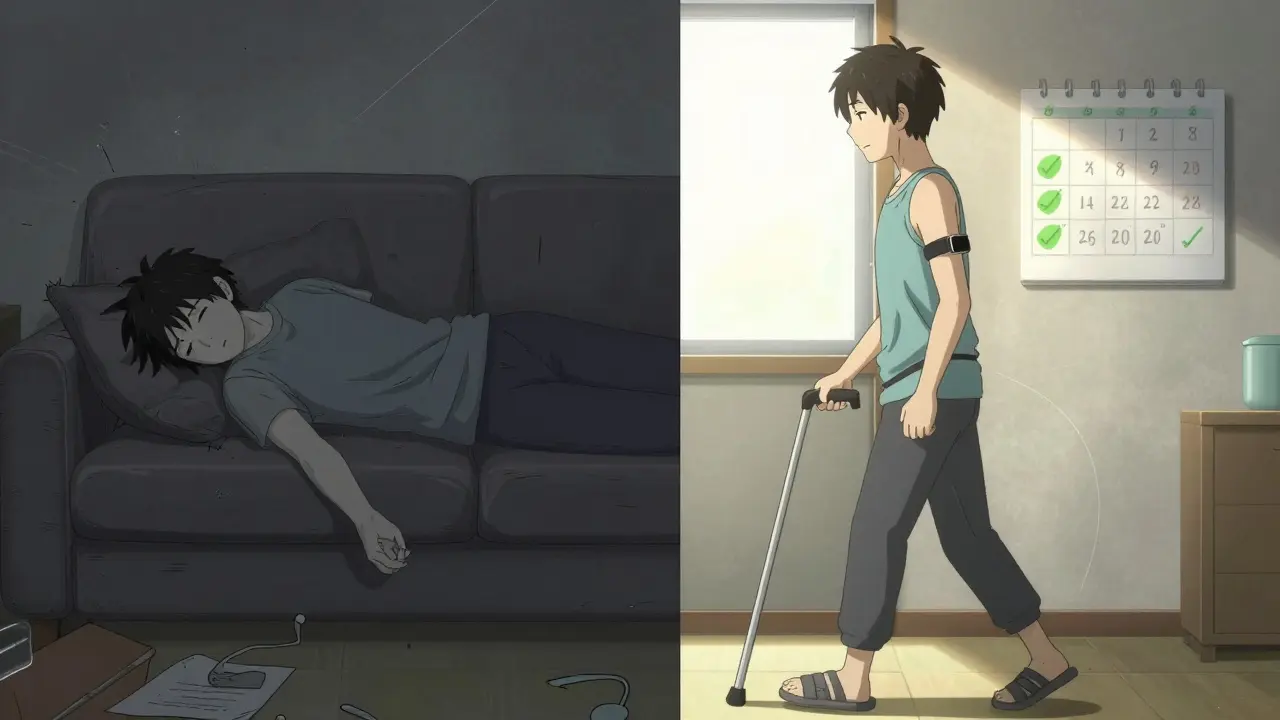
Getting the Right Care
Not every physical or occupational therapist knows how to handle autoimmune disease. Look for someone with specialized training. The Academy of Pelvic Health Physical Therapy offers a 120-hour Autoimmune Specialty Certification. Only 78% pass. That’s your benchmark. Ask your therapist: “Do you have training in autoimmune conditions?” “Do you adjust therapy based on flare vs. remission?” “Do you use the HAQ-DI or COPM to track progress?” If they hesitate, keep looking. Insurance is another hurdle. In 31 U.S. states, there’s no specific billing code for autoimmune rehab. That means 22% of claims get denied. Many plans cap sessions at 12-15 per year-even though experts recommend 24-30 to see lasting results.What’s New in 2026
The field is evolving fast. The NIH’s Autoimmune Rehabilitation Registry, launched in 2023, tracks outcomes for over 5,000 patients. New research shows that adjusting exercise intensity based on weekly blood markers like IL-6 improves outcomes by 39%. That’s huge. AI tools are coming. The Lupus Foundation’s ‘PacePartner’ app, in Phase 3 trials, uses wearable data to predict flares with 82% accuracy. It tells you: “Your heart rate variability dropped 15% overnight. Rest today.” Medicare increased reimbursement for chronic condition rehab by 5.7% in 2024. That’s good news. But there’s a looming crisis: by 2026, the U.S. will be short 18,000 trained therapists. If you’re getting care now, hold onto it. It’s not easy to replace.Your Next Steps
If you’re struggling with daily tasks because of your autoimmune disease:- Ask your rheumatologist for a referral to a therapist with autoimmune training.
- Start with an assessment using HAQ-DI or COPM. Know your baseline.
- Insist on therapy that adjusts to your flare-ups-not one that pushes through them.
- Learn the 70% rule. Track your energy. Use a simple notebook or app.
- Explore adaptive tools. A $20 jar opener or voice assistant can change your life.
- If insurance denies coverage, appeal. Cite the 2022 Journal of Autoimmunity and ACR guidelines.
Can I do rehab during a flare-up?
Yes-but only with modified, low-intensity movements. During a flare, avoid stretching, high-impact activity, or anything that increases joint heat or swelling. Focus on gentle isometric exercises, breathing techniques, and rest. Pushing through pain can make flares last longer. Always check with your therapist before continuing.
How long does it take to see results from rehab?
Most people notice small improvements in energy and pain within 4-6 weeks. Meaningful gains in daily function-like being able to dress yourself or cook meals-typically appear after 3-6 months of consistent therapy. The key is sticking with it, even on good days. Progress isn’t linear, but it’s real.
Is hydrotherapy better than regular exercise?
For people in active disease phases, yes. Hydrotherapy reduces pain by 22% more than land-based exercise and is easier on swollen joints. But if you don’t have access to a pool, land-based aerobic exercise at low intensity still works. The goal isn’t the environment-it’s consistent, paced movement.
What if my therapist doesn’t understand my fatigue?
That’s a red flag. Central fatigue is real and common in lupus, Sjögren’s, and fibromyalgia. If your therapist dismisses your exhaustion as “lack of motivation,” find someone new. Look for therapists who use heart rate variability monitoring or ask about your energy levels daily. Your fatigue isn’t weakness-it’s a signal.
Can occupational therapy help with cognitive issues?
Yes. Many autoimmune diseases cause brain fog. OTs help by simplifying tasks: using checklists, setting phone reminders, reducing clutter, and breaking tasks into smaller steps. They also recommend tools like voice-to-text apps or smart calendars. Managing cognitive load is part of restoring independence.
Are home-based rehab programs effective?
Very. Since 2020, 68% of patients use telehealth rehab, and outcomes match in-person care when programs are personalized. Look for programs that include video check-ins, activity tracking, and therapist feedback. Avoid apps that just show generic exercises. Your plan must adapt to your daily symptoms.


Comments
Candice Hartley January 26, 2026 AT 13:21
I just started OT last month and already I can hold a coffee cup without my fingers screaming. 🙌 That one-handed can opener? Lifesaver.
Kathy McDaniel January 26, 2026 AT 15:27
the 70% rule changed my life honestly i used to think i was lazy but no its just my body being smart lol
Conor Flannelly January 28, 2026 AT 09:06
There’s a quiet dignity in learning to move within limits. It’s not about pushing past pain-it’s about honoring the body’s wisdom. The water doesn’t judge you for needing its support. It just holds you. And in that holding, you rebuild-not the body you had, but the life you still can live. This isn’t rehab as a fix. It’s rehab as a homecoming.
John O'Brien January 28, 2026 AT 20:09
my PT told me to do underwater treadmills and i thought she was crazy until i tried it. i cried the first time i walked without pain. 6 months later i’m gardening again. fuck yeah rehab.
Anjula Jyala January 29, 2026 AT 15:08
HAQ-DI and COPM are gold standards but most therapists dont even know what they are. You need to demand evidence based practice not generic stretching routines. Your fatigue is not weakness its immunometabolic dysregulation. Stop accepting bandaid solutions
Kegan Powell January 30, 2026 AT 00:45
you guys are right about the 70% rule. i used to think i was failing because i couldn't do everything. now i track my HRV with my apple watch and if it drops 10% i rest. no guilt. no shame. just smart pacing. this isn't a race it's a lifelong dance with your body
Conor Murphy January 30, 2026 AT 11:15
my sister has lupus and she got a voice-activated home system last year. she said turning on the lights with her voice made her feel human again. small things matter so much.
Marian Gilan January 31, 2026 AT 13:31
they told me to tough it out and now i’m on disability. 19% of therapists don’t even know central fatigue is real. who’s running these programs? the same people who think chronic pain is just in your head? i swear if one more person says ‘just exercise more’ i’m gonna scream
Desaundrea Morton-Pusey February 1, 2026 AT 14:55
why are we even talking about rehab? the real problem is the government won’t fund proper care. this is all just a bandaid. we need universal healthcare that covers this stuff without 12 appeals. this is capitalism failing people with chronic illness.
Patrick Merrell February 2, 2026 AT 16:07
hydrotherapy works because water is nature’s anti-inflammatory. it’s not magic. it’s physics. and if your therapist doesn’t get that, they’re just selling you a spa day. real rehab is science not vibes
Murphy Game February 3, 2026 AT 12:19
the NIH registry? 5000 patients? sounds like a controlled experiment. but who’s funding it? big pharma? the same companies that make the drugs that cause the fatigue? they’re not helping you. they’re monetizing your suffering. watch the video on YouTube called ‘Rehab Lies’