Most people don’t realize that hepatitis B and hepatitis C are two of the most common viral liver infections on the planet. Together, they affect over 350 million people worldwide. And yet, many still don’t know how they’re passed on, whether they can be tested for easily, or if there’s even a cure. The good news? Science has made huge leaps in the last decade. The bad news? Too many people still don’t get tested or treated - and that’s costing lives.
How Hepatitis B and C Spread - And What Doesn’t Spread Them
Hepatitis B and C don’t spread the same way. Knowing the difference could save your life - or someone else’s.Hepatitis B is incredibly contagious. It moves through blood and bodily fluids. That means sex without a condom, sharing needles, or even a razor or toothbrush with an infected person can pass it along. If you’re born to a mother with hepatitis B, you’re at high risk - up to 90% of babies infected at birth develop chronic infection if not treated immediately. Healthcare workers, people who inject drugs, and men who have sex with men are at higher risk. But here’s what you need to hear: you cannot catch hepatitis B from hugging, sharing food, coughing, or using the same toilet. It’s not airborne. It’s not casual.
Hepatitis C spreads almost exclusively through blood. The biggest driver today? The opioid crisis. In the U.S., cases among people aged 20 to 39 have jumped 71% since 2014. Sharing needles, syringes, or even dirty straws for snorting drugs is the main route. It can also pass from mother to baby during childbirth - about 5 to 6% of the time. Unlike hepatitis B, hepatitis C is not spread through sex under normal circumstances, unless there’s blood involved - like during rough sex or if someone has an STI.
Who Should Get Tested - And When
Testing is the first step to stopping these viruses. But too many people never get checked.The CDC now recommends everyone over 18 get tested for hepatitis C at least once - no exceptions. Pregnant women should be tested during every pregnancy. If you’ve ever injected drugs, even once, or got a tattoo in an unregulated place, you need a test. People with HIV have a 70-90% chance of also having hepatitis C. That’s why co-testing is standard.
For hepatitis B, the rules are stricter. Everyone should be screened at least once in their life. But if you’re from a region where hepatitis B is common - like parts of Asia, Africa, or Eastern Europe - you’re at higher risk. So are healthcare workers, people on dialysis, and anyone starting chemotherapy. If you’re pregnant, your doctor should test you for hepatitis B during your first visit. If you’re positive, your baby gets a shot within 12 hours of birth - that cuts infection risk by 95%.
Testing for hepatitis B requires a blood panel: HBsAg tells you if you’re currently infected, anti-HBs shows you’re immune (from vaccine or past infection), and HBV DNA measures how much virus is in your blood. For hepatitis C, it starts with an antibody test. If that’s positive, you need a second test - HCV RNA - to confirm the virus is still active. About 44% of people with hepatitis C don’t know they have it. That’s why testing is so critical.
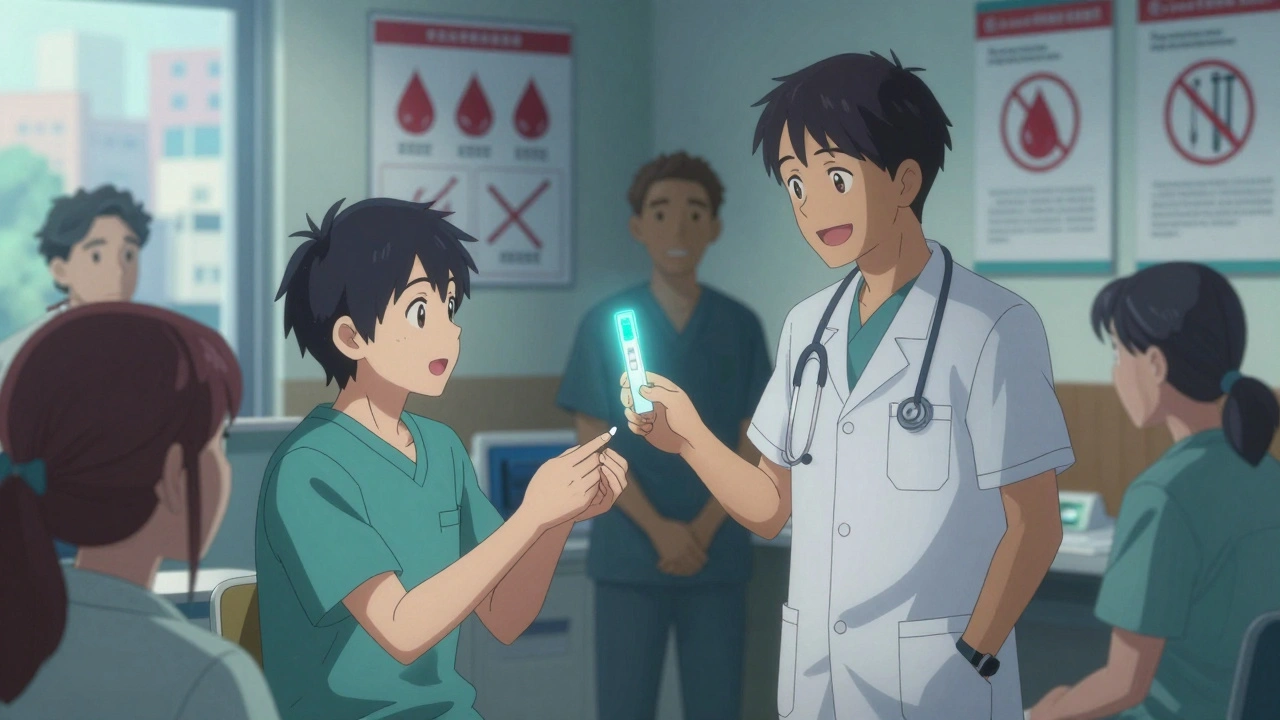
Testing Advances: Faster, Cheaper, Easier
The old days of waiting weeks for lab results are fading.Today, there are point-of-care tests that give results in minutes. The OraQuick HCV test, approved by the FDA in 2010, uses a finger prick and shows results in under 20 minutes. For hepatitis B, new rapid tests are hitting clinics with 98.5% accuracy. These aren’t just for big hospitals - community health centers, mobile vans, and even pharmacies in rural areas are using them.
In Egypt, a national campaign used these tests to screen 75 million people between 2018 and 2021. They found over 3 million cases and treated nearly all of them. Hepatitis C prevalence dropped from 14.7% to 0.9%. That’s not science fiction - it’s real, and it’s replicable.

Treatment for Hepatitis C: The Cure Is Here
If you’re living with hepatitis C, the news is better than ever.Before 2011, treatment meant weekly injections of interferon, side effects so bad people quit, and cure rates under 50%. Now? Direct-acting antivirals (DAAs) like Epclusa and Mavyret cure more than 95% of cases. They’re pills. Taken once a day. For 8 to 12 weeks. No needles. No fatigue. No depression.
These drugs work against all six major strains of hepatitis C. They’re so effective, the WHO now calls elimination of hepatitis C a realistic goal by 2030. The problem? Access. In the U.S., a full course of DAAs cost $84,000 in 2014. Today, it’s $24,000 to $30,000. But in India or Egypt, generic versions cost less than $300. That’s the gap. And it’s why millions still go untreated.
Doctors are now training nurses and pharmacists to manage treatment - no liver specialist needed. This “task-shifting” is making cure possible in places that never had access before.
Treatment for Hepatitis B: No Cure Yet - But Better Control
Hepatitis B is trickier. There’s no pill that clears the virus completely - yet.Current treatments - like tenofovir alafenamide (TAF) and entecavir - don’t cure. They suppress. They stop the virus from damaging your liver. Most people need to take them for life. The good news? These drugs are safer than older versions. TAF causes less kidney and bone damage. They’re also highly effective at lowering viral load, which means you’re far less likely to pass it on.
There’s hope on the horizon. In 2025, over 20 new drugs are in late-stage trials. Some, like JNJ-3989 (an siRNA therapy), aim to knock down the virus’s ability to hide in liver cells. Others, like capsid modulators, disrupt how the virus builds itself. Therapeutic vaccines are being tested to train the immune system to fight back. A few patients - 3 to 7% - have achieved what’s called a “functional cure”: they lose HBsAg and develop protective antibodies. It’s rare, but it’s happening.
The 2025 Guidelines Update says doctors should now consider treating adolescents with high viral loads - even if they feel fine - if they have a family history of liver cancer or have diabetes or fatty liver disease. That’s a shift. We’re no longer waiting for damage to show up.
The Vaccine That Works - And Why It’s Still Underused
Hepatitis B is the only major viral hepatitis with a vaccine. It’s been around since 1986. It’s safe. It’s effective. It lasts for life.Yet in the U.S., only 66.5% of adults have completed the full 3-dose series. That’s far below the 90% target. Why? A mix of misinformation, lack of awareness, and gaps in healthcare access. Many think, “I’m not at risk,” or “I got it as a kid.” But hepatitis B can strike anyone. It’s why the CDC now recommends universal adult vaccination.
The real game-changer is the birth dose. If every newborn gets the first shot within 24 hours of birth, we could eliminate mother-to-child transmission. That’s the key to ending hepatitis B in 20 years. But globally, only 43% of babies get that first shot on time. In low-income countries, the gap is even wider.
What’s Holding Us Back - And What’s Being Done
We have the tools. We have the science. So why are hepatitis B and C still killing over a million people a year?Three things: stigma, cost, and lack of screening.
People still feel ashamed if they have hepatitis C - especially if they injected drugs. That shame keeps them from getting tested. Cost blocks access. Even with insurance, co-pays for hepatitis B drugs can hit $500 a month. And without routine testing, infections go unnoticed until the liver is badly damaged.
But change is happening. In Scotland, free testing and treatment are now offered in drug support centers. In Canada, provinces are covering DAAs for everyone, regardless of liver damage. In the U.S., Medicaid expansion in 38 states now covers hepatitis C treatment without restrictions. That’s progress.
The WHO’s 2030 goals - 90% fewer new infections, 65% fewer deaths - are ambitious. But Egypt proved they’re possible. With the right investment in testing, treatment, and education, we can make hepatitis B and C rare diseases - not global threats.
What You Can Do Right Now
You don’t need to wait for a policy change. Here’s what you can do today:- If you’re over 18, get tested for hepatitis C. One blood test. That’s it.
- If you’ve never been vaccinated for hepatitis B, ask your doctor. It’s three shots over six months. Free or low-cost at most public health clinics.
- If you’re pregnant, make sure your OB tests you for hepatitis B.
- If you use drugs, don’t share needles. Use clean ones. Many pharmacies give them out for free.
- If you’re positive, tell your close contacts. They need testing too.
These viruses don’t care about your income, your job, or your background. They only care if you’re exposed. But now, we have the power to stop them. All it takes is knowing - and acting.
Can you get hepatitis B from kissing?
No, hepatitis B is not spread through kissing, hugging, or sharing utensils. The virus isn’t present in saliva in enough quantity to cause infection. Transmission requires blood or bodily fluids - like through sex, sharing needles, or from mother to baby during birth.
Is hepatitis C curable?
Yes. Modern direct-acting antiviral (DAA) medications cure over 95% of hepatitis C cases. Treatment usually lasts 8 to 12 weeks and has few side effects. Once cured, the virus is gone from your body and you can’t pass it on.
Do I need to get tested for hepatitis B if I was vaccinated as a child?
If you completed the full 3-dose vaccine series as a child, you’re likely protected for life. But if you’re at high risk - like a healthcare worker, someone with multiple sexual partners, or from a high-prevalence country - your doctor may check your antibody levels (anti-HBs) to confirm immunity.
Can hepatitis B turn into hepatitis C?
No. Hepatitis B and hepatitis C are caused by completely different viruses. One cannot turn into the other. But it’s possible to be infected with both at the same time - especially if you’ve had multiple exposures through blood or needles. Co-infection can speed up liver damage, so testing for both is important.
Are generic hepatitis C drugs safe?
Yes. Generic versions of sofosbuvir and other DAAs, made in countries like India and Egypt under WHO guidelines, have the same active ingredients and effectiveness as brand-name drugs. Studies show cure rates above 95%, matching clinical trial results. They’re a major reason why countries like Egypt have slashed hepatitis C rates.
How often should I get tested if I’m at risk?
If you inject drugs, have multiple sexual partners, or are HIV-positive, get tested every 6 to 12 months. If you’re pregnant, test once during pregnancy. For most adults, one-time testing for hepatitis C is enough - unless your risk changes. For hepatitis B, if you’re unvaccinated, get tested once. If you’re vaccinated, you usually don’t need repeat testing unless you’re in a high-risk group.

Comments
ruiqing Jane December 3, 2025 AT 11:31
Just got tested for HCV yesterday-negative. But I’m telling everyone I know to do the same. One blood test, 10 minutes of your life, and you could save yourself from decades of liver damage. Seriously, if you’re over 18 and haven’t been tested, stop scrolling and call your doctor today.
I’m not being dramatic. This is the easiest life-saving move you’ll ever make.
And if you’re on the fence about the HBV vaccine? Get it. It’s safe. It’s free at most clinics. And it lasts a lifetime. No excuses.
Fern Marder December 4, 2025 AT 04:21
OMG YES 🙌 I got cured of HCV last year with Mavyret. 8 weeks. No side effects. Just took a pill before bed. Now I’m 100% virus-free and my liver enzymes are normal. I used to be too ashamed to talk about it because I used to inject drugs years ago… but now I’m shouting it from the rooftops. If you have it, get treated. You’re not broken. You’re just overdue for a miracle. 💪❤️
Carolyn Woodard December 5, 2025 AT 09:38
It’s fascinating how the molecular biology of HBV versus HCV dictates such divergent clinical trajectories. HBV integrates into the host genome via covalently closed circular DNA (cccDNA), which creates a persistent reservoir that current nucleos(t)ide analogs cannot eradicate-hence the need for lifelong suppression. In contrast, HCV exists solely as an RNA virus with no genomic integration, making direct-acting antivirals capable of achieving virologic cure by targeting NS3/4A, NS5A, and NS5B with near-perfect specificity.
What’s more intriguing is the immunological paradox: HBV induces immune tolerance in early infection, whereas HCV often triggers a robust but ultimately ineffective cytotoxic T-cell response. This explains why therapeutic vaccines for HBV are so challenging to develop, while HCV cure rates are now >95%.
Yet the real barrier isn’t science-it’s socioeconomic determinants. The 2025 WHO elimination targets will remain aspirational until we decouple treatment access from profit-driven pharmaceutical monopolies. Generic DAAs cost $300 in India. Why are they $30,000 here? The answer isn’t pharmacological. It’s political.
Allan maniero December 6, 2025 AT 14:58
I’ve been working in public health in rural Kentucky for 12 years, and let me tell you-this article nails it. We’ve got mobile vans hitting backroads now with rapid HCV tests. People who’ve never set foot in a clinic in 20 years are walking in because the nurse says, ‘It’s just a finger prick, no judgment.’
One woman, 62, never knew she had it. Her husband died of liver cancer last year. She got tested after his funeral. Turned out she’d had HCV since the ‘80s, from a blood transfusion. She’s on treatment now. Her kids are getting vaccinated for HBV. That’s the ripple effect.
It’s not about fancy tech. It’s about meeting people where they are. And honestly? We’re finally doing that.
william tao December 8, 2025 AT 02:13
Let’s be clear: this is a textbook case of medical paternalism disguised as public health. Mandatory testing for everyone over 18? That’s not prevention-it’s surveillance. And the fact that we’re now pushing universal HBV vaccination for adults suggests a fundamental failure of risk-based screening. Why not just test the high-risk groups? Why force everyone into the system? It’s inefficient, invasive, and frankly, a slippery slope toward mandatory medical compliance.
Also, the claim that DAAs are ‘safe’ ignores the long-term data. We’ve only had them since 2011. Are we really sure there aren’t latent autoimmune or neurotoxic effects decades down the line? I think we’re rushing to declare victory before we’ve even finished the study.
Sandi Allen December 8, 2025 AT 10:27
WAIT. WAIT. WAIT. So you’re telling me the government wants me to get a blood test for HCV… and then they’re going to tell me I have it… and then they’re going to make me take pills… and then they’re going to track me… and then they’re going to tie my insurance to my liver status… and then they’re going to start asking about my drug use… and then they’re going to call child services if I have kids… and then they’re going to take away my freedom??
THIS IS A SNAKE OIL SCHEME. THE PHARMA COMPANIES ARE PUSHING THIS TO MAKE MONEY. THE VACCINE ISN’T SAFE-IT’S FULL OF ALUMINUM AND FORMALDEHYDE. AND THE ‘CURE’ FOR HCV? IT’S A LIE. THEY JUST MASK THE VIRUS. THEY’RE LYING TO YOU.
DO YOUR OWN RESEARCH. CHECK OUT THE VAXXED DOCUMENTARY. THEY’RE HIDING THE TRUTH. I’M NOT GETTING TESTED. I’M NOT TAKING PILLS. I’M NOT PLAYING THEIR GAME.
Sheryl Lynn December 10, 2025 AT 04:46
How delightfully quaint-this piece reads like a WHO press release written by a particularly earnest intern who just finished reading ‘The Emperor of All Maladies’.
Yes, yes, DAAs are miraculous. Yes, yes, Egypt’s program is laudable. But let’s not pretend this is a triumph of public health-it’s a triumph of market liberalization in the Global South, where generics are manufactured under looser regulatory frameworks and labor costs are negligible.
Meanwhile, in the West, we’ve turned hepatitis C into a luxury commodity: a $30K pill for the privileged, a death sentence for the uninsured. The real innovation here isn’t pharmacological-it’s the art of selling hope while pricing out the very people who need it most.
And don’t even get me started on the HBV vaccine. It’s not underused because of ‘misinformation.’ It’s underused because the medical establishment has spent decades treating it like a ‘minor’ issue-while quietly letting the virus fester in immigrant communities, then patting themselves on the back for ‘universal screening’ when the damage is done.
It’s not science that’s failing us. It’s capitalism.
Paul Santos December 10, 2025 AT 20:26
Interesting how we romanticize Egypt’s success while ignoring the cultural and structural conditions that made it possible: centralized healthcare, state-led mobilization, and a population that trusts public institutions. Here? We’ve got fragmented care, distrust of authorities, and a system where your insurance provider decides if you get treated based on your fibrosis score.
And yet, we still act like the problem is individual ignorance. ‘Just get tested!’ they say. As if the answer to systemic collapse is a pep talk.
Also, I’m still waiting for someone to explain why the CDC recommends testing everyone over 18 for HCV but not for hepatitis A-which is just as transmissible and far more common in food service workers. Hypocrisy much?
Anyway. I got my HCV test last year. Negative. Still got the HBV vaccine. Still paranoid about shared toothbrushes. 😅
Eddy Kimani December 11, 2025 AT 08:55
Just want to add a data point: in my clinic, we’ve started using point-of-care HBV tests for patients on dialysis. We used to wait 3 weeks for lab results. Now we get results in 15 minutes. One guy, 58, came in for a routine check-positive for HBsAg. We started him on TAF that same day. His viral load dropped from 8 million IU/mL to undetectable in 12 weeks. No side effects.
And the best part? He told his sister. She got tested. She was positive too. We got her on treatment. Now her kids are getting vaccinated.
This isn’t just about medicine. It’s about breaking chains of transmission. One test. One pill. One conversation. That’s all it takes.