Splitting or crushing pills might seem like a simple fix-maybe you’re trying to save money, make a pill easier to swallow, or adjust a dose for an elderly loved one. But what looks like a small convenience can turn into a serious health risk if done wrong. Contamination, uneven doses, and exposure to dangerous chemicals aren’t just theoretical risks-they’ve caused real harm. In 2023, a single shared pill splitter in a care home led to 14 residents getting accidental warfarin overdoses. That’s not an outlier. It’s a warning.
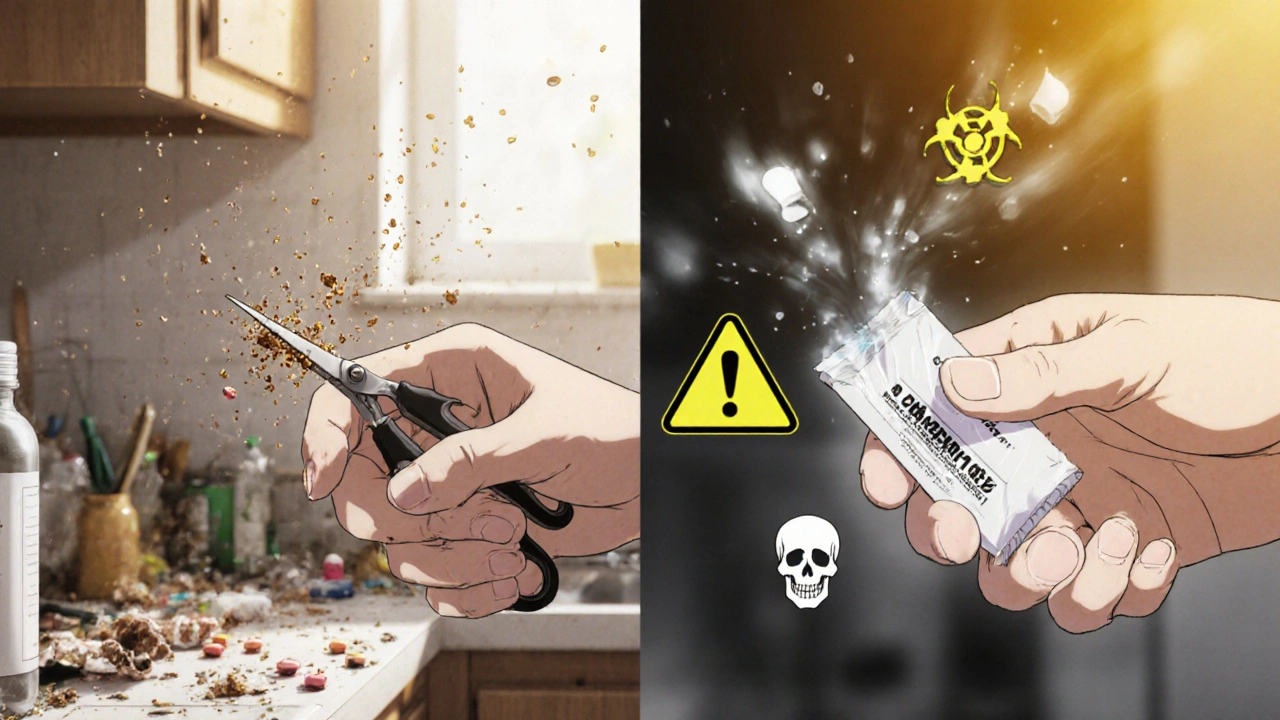
Why Contamination Happens (And Why It’s Dangerous)
Pills aren’t just little chunks of medicine. Many are built with special coatings or timed-release layers. When you crush or split them improperly, you’re not just changing the shape-you’re breaking the science behind how the drug works. And worse, you’re spreading residue.Take a pill like cyclophosphamide, used in cancer treatment. It’s a hazardous drug. Even tiny amounts left on a splitter or in a crusher can stick to your skin, get into the air, or transfer to another person’s medication. Studies have found traces of this drug on caregivers’ gloves at levels high enough to cause harm. A 2019 study showed 4.7 ng/cm² of cyclophosphamide on gloves after crushing without a closed system. That’s enough to affect bone marrow and increase cancer risk over time.
Even non-hazardous pills can cross-contaminate. If you crush a blood pressure pill and then use the same device for an antibiotic, you’re mixing drugs. That’s not just ineffective-it’s dangerous. People with heart conditions, kidney issues, or allergies can have severe reactions to even small amounts of the wrong medication.
Which Pills Should Never Be Split or Crushed
Not all pills are created equal. The FDA estimates that 97.8% of enteric-coated, extended-release, or sustained-release medications should never be split or crushed. Here’s what to watch for:- Enteric-coated pills-These have a special coating to protect your stomach or delay absorption until the pill reaches the intestine. Crushing them can cause nausea, vomiting, or stomach ulcers.
- Extended-release (ER), sustained-release (SR), or controlled-release (CR)-These are designed to release medication slowly over hours. Crushing them releases the full dose at once, which can lead to overdose. Examples include OxyContin, Metformin ER, and Adderall XR.
- Capsules with beads-Many capsules contain tiny beads that release medication over time. Opening them destroys this system.
- Hazardous drugs-Cancer meds, immunosuppressants, and some psychiatric drugs. These require closed-system crushing only.
Look for labels like “do not crush,” “swallow whole,” or “extended-release.” If you’re unsure, ask your pharmacist. Never guess.
The Right Tools for the Job
Using scissors, a knife, or your fingers to split a pill is risky. These methods lead to uneven doses and leave behind residue. A 2021 study found that manual splitting resulted in dose variations of up to 36%-far beyond the 5% safety threshold for most medications.Use a dedicated pill splitter with a v-shaped holder and a stainless steel blade. Look for models with retractable blades and a clear cover to contain dust. The Silent Knight pill crusher is the gold standard for hazardous drugs-it traps 99.8% of particles in a sealed chamber, according to NIOSH testing. For non-hazardous pills, a simple splitter like the Med-Plus Pro (2024 model) includes visual alignment guides to help you center the pill correctly.
Never share equipment between patients or medications. Even if you wipe it down, residue can remain. One study found that 68% of shared splitters still had detectable traces of medication after cleaning with water alone.

Step-by-Step Safe Splitting and Crushing Protocol
Follow these steps every single time. Skipping one can put someone at risk.- Wash your hands thoroughly with soap and water. Wear disposable nitrile gloves-latex doesn’t block chemical residue.
- Check the pill. Confirm it’s safe to split or crush using the label or by asking a pharmacist. Look for a score line-only split pills with a clear, centered groove.
- Disinfect your tools. Wipe the splitter or crusher with a 70% isopropyl alcohol wipe. Let it air dry. Do this before every use, even if it’s the same person’s pill.
- Split one pill at a time. Don’t split your whole month’s supply. Split pills lose potency faster. Store split pills in a dry, cool place and use within 24 hours.
- Use a closed system for hazardous drugs. Only use FDA-cleared, sealed crushers like the Silent Knight. Never crush these in open containers.
- Dispose of residue properly. Wipe the inside of the splitter with a damp cloth and throw the cloth in a sealed trash bag. Don’t rinse it down the sink.
- Administer immediately. Don’t leave split or crushed pills sitting out. Some medications degrade when exposed to air or moisture.
What Not to Do
Here are common mistakes-and why they’re dangerous:- Using scissors or a knife-Leaves uneven pieces and sharp edges that can cut your fingers or leave behind drug residue.
- Sharing splitters between people-Causes cross-contamination. One 2023 survey found 41.7% of home caregivers didn’t know this was a risk.
- Cleaning with water only-Water doesn’t remove chemical residue. Alcohol wipes are required.
- Splitting pills without a score line-Most pills without a groove aren’t designed to split. You’re guessing the dose.
- Storing split pills for days-Oxygen and moisture break down the medication. Potency drops fast.
Who’s at Risk? And Who Shouldn’t Be Splitting Pills
This isn’t just a problem in nursing homes. Over 23% of long-term care residents in the U.S. need split doses. But it’s also happening at home. With rising medication costs and telehealth visits, more people are splitting pills without proper guidance.People most at risk:
- Older adults swallowing large pills
- Children needing smaller doses
- Patients on expensive medications trying to stretch supplies
- Caregivers without training
But here’s the hard truth: if you’re not trained, you shouldn’t be doing it. A 2022 study showed that pharmacist-led education reduced splitting errors by 58.3%. That means a 10-minute chat with your pharmacist can prevent a life-threatening mistake.
What You Can Do Right Now
You don’t need to wait for a policy change. Start today:- Ask your pharmacist: “Is this pill safe to split or crush?” Write down their answer.
- Buy a dedicated pill splitter-costs under $15. Look for one with a clear cover and a blade guard.
- Keep alcohol wipes next to your pill splitter. Use them every time.
- Label your splitter with the resident’s name if you’re in a care setting.
- Never crush hazardous drugs unless you have a closed-system crusher.
- If you’ve been splitting pills the wrong way, stop. Talk to your doctor or pharmacist about alternatives-like liquid forms or lower-dose tablets.
Medication safety isn’t about being perfect. It’s about being consistent. One clean splitter, one wipe, one pill at a time-those small actions prevent big disasters.
Emerging Solutions
The future is getting smarter. New FDA-cleared devices like the Med-Engage splitter (2024) use sensors to verify the pill is centered and confirm the split was even. These tools connect to electronic health records and flag unsafe splits in real time. Hospitals are starting to use them. Eventually, they’ll be available for home use too.For now, stick to the basics: the right tool, the right technique, and the right mindset. Don’t treat pills like snacks. Treat them like precision medicine-because that’s what they are.
Can I split a pill without a score line?
No. Pills without a score line weren’t designed to be split. The active ingredient may not be evenly distributed, and you risk creating uneven or dangerous doses. Even if the pill looks like it should split, don’t do it unless your pharmacist confirms it’s safe.
Is it safe to crush pills for a feeding tube?
Only if the medication is explicitly approved for crushing and tube administration. Many pills, especially extended-release or enteric-coated ones, will clog the tube or release too much drug at once. Always check with your pharmacist before crushing any pill for a feeding tube. Some medications come in liquid or sprinkle forms designed for this purpose.
How often should I clean my pill splitter?
Clean it with a 70% isopropyl alcohol wipe before every use-even if it’s the same person’s pill. Residue from one medication can transfer to another. Water or a dry cloth isn’t enough. Alcohol wipes are the minimum standard for contamination control.
Can I reuse the same pill splitter for multiple people?
Never. Each person should have their own dedicated splitter. Sharing-even with cleaning-creates a high risk of cross-contamination. In care homes, this has led to outbreaks of unintended drug reactions. Label each splitter with the resident’s name to avoid mix-ups.
What should I do if I’ve already split or crushed a pill that shouldn’t have been?
Stop using it immediately. Don’t give it to anyone. Contact your pharmacist or healthcare provider right away. They can advise whether the medication is still safe, if a replacement is needed, or if any monitoring is required. If the pill was a hazardous drug, report the incident to your facility’s safety officer.
Are there alternatives to splitting or crushing pills?
Yes. Many medications come in lower-strength tablets, liquids, or chewable forms. Ask your doctor or pharmacist if a different formulation is available. For example, instead of splitting a 20mg tablet, you might get two 10mg tablets. Or switch to a liquid version. These options are often safer and more accurate than splitting.

Comments
Holli Yancey November 18, 2025 AT 14:33
My grandma takes five pills a day and can't swallow the big ones. I started using a cheap splitter from Walmart until I read this. Now I buy alcohol wipes every time I split her meds. Small habit, huge difference.
Jessica Healey November 18, 2025 AT 22:20
Y’all act like this is news. My aunt crushed her antidepressant because she thought it’d work faster. Ended up in the ER. Don’t be that person.
Joseph Peel November 19, 2025 AT 04:23
Pharmacists are the unsung heroes of medication safety. I’ve had mine walk me through pill splitting three times this year. Never guess. Always ask. It’s literally that simple.
Kyle Swatt November 19, 2025 AT 13:05
People treat pills like snacks like they’re chips from a bag. But a pill ain’t a snack-it’s a precision instrument. Crush it wrong and you’re not just wasting money, you’re playing Russian roulette with someone’s heart, brain, or bone marrow. I’ve seen it. It ain’t pretty. That 4.7 ng/cm² stat? That’s not a number. That’s a ghost haunting a caregiver’s gloves. We don’t need more tech. We need more damn respect.
Shannon Hale November 19, 2025 AT 15:13
Oh wow, another ‘pharmaceutical industry wants you scared’ article. Newsflash: 99% of people who split pills live to tell the tale. You’re scaring grandmas into swallowing whole pills they can’t choke down. What’s the real risk? The fear-mongering. The Silent Knight? $300? For what? A glorified meat grinder? I split pills with a butter knife since 2008. Still breathing. Still sane.
Tarryne Rolle November 20, 2025 AT 23:25
So… you’re saying the FDA and Big Pharma are the only ones who know how to handle pills? What about the millions of people who’ve been splitting meds for decades without incident? This feels like a corporate ploy to sell $200 ‘medical-grade’ splitters. I’ll take my kitchen scissors and my common sense thank you very much.
Gordon Mcdonough November 21, 2025 AT 02:02
AMERICA IS BEING POISONED BY OVERREGULATION. I split my dad’s blood pressure pill with a pocketknife. He’s 82. He’s alive. The government wants you to pay for a $50 gadget so they can track you. This is socialism disguised as safety. Let people live. Let people split pills. If you’re scared, don’t do it. But don’t force your fear on the rest of us. Also, the word ‘cyclophosphamide’ is spelled wrong here. I know because I used to work in oncology. And I didn’t need no ‘closed system’.
Levi Hobbs November 21, 2025 AT 23:01
Just wanted to say thank you for this. My mom’s on warfarin and I used to split her pills with my fingers. I had no idea how dangerous that was. I bought the Med-Plus Pro yesterday. Cleaned it with alcohol. Split one pill. Felt like I just performed surgery. But it felt right. I’m not scared anymore-I’m careful. That’s the difference.
henry mariono November 22, 2025 AT 22:18
My sister works in hospice. She told me about a case where a nurse used the same crusher for chemo and diabetes meds. One patient had a seizure. No one knew why until they tested the device. It’s not paranoia. It’s protocol. I’ve started labeling my splitter with my name. Small thing. Big safety net.
Prem Hungry November 24, 2025 AT 10:59
From India, where we split pills with teeth because no one can afford splitters. But I agree-this is vital knowledge. My uncle died from a crushed extended-release tablet. Please, if you are reading this, do not gamble with medicine. Even if you cannot afford tools, ask your pharmacist for liquid forms. They are often cheaper than you think. Safety is not a luxury. It is a right.
Jeremy Hernandez November 24, 2025 AT 17:34
THIS IS A GOVERNMENT PSYOP. The FDA doesn’t care about your safety-they care about liability. They know people are splitting pills because they can’t afford meds. So they scare you into buying expensive gadgets. Meanwhile, the price of OxyContin hasn’t dropped. The real villain isn’t the knife-it’s the pharmaceutical cartel. Also, I crushed my Adderall XR once. Felt amazing. No side effects. So there.
Bill Machi November 24, 2025 AT 22:10
Look, I’m not a doctor. But I’ve been splitting my dad’s meds for six years. I wipe the splitter with a paper towel. He’s 79. He’s alive. I’ve read this entire article. It’s 12 pages of fear. Where’s the data on how many people die from NOT splitting pills because they’re too scared? You’re creating a new kind of harm. People skip doses. People go without. That’s the real epidemic. Not the splitter. The silence. The shame. The guilt. Stop scaring people. Start helping them.
Sridhar Suvarna November 24, 2025 AT 22:17
As someone from India who has seen both worlds-where pills are split with bare hands and where hospitals use sealed crushing systems-I can say this: safety is not about wealth. It is about awareness. A single alcohol wipe costs less than a cup of tea. A dedicated splitter costs less than a phone charger. The cost is not the barrier. The ignorance is. Education, not equipment, is the true solution. Thank you for writing this. Please share it with every caregiver, every grandchild, every home.