When you pick up a prescription, you might see a pop-up on the pharmacist’s screen: "Allergy Alert: Penicillin". It sounds serious. But what does it actually mean? Is this a real danger-or just noise in the system? Most people assume these alerts are flawless safety nets. The truth is, they’re often wrong. And if you don’t know how to read them, you could be missing real risks-or ignoring warnings that matter.
What You’re Seeing Isn’t Always an Allergy
Pharmacy allergy alerts come from electronic health records (EHRs) like Epic or Cerner. They compare what’s being prescribed to what’s been entered as an allergy in your file. But here’s the catch: a lot of what’s entered isn’t an allergy at all. People write down "penicillin allergy" because they got a stomach ache after taking it as a kid. Or they had a rash after amoxicillin that turned out to be a virus. Or they were told they were allergic without ever being tested. A 2019 study in the Annals of Allergy, Asthma & Immunology found that only 12% of NSAID allergy alerts actually represented real allergic reactions. For penicillin, the most common alert, fewer than 2% of people who think they’re allergic are truly allergic. Yet, 89% of EHR systems still treat every "penicillin allergy" as a life-threatening warning. The system doesn’t know the difference between a true immune reaction (like hives, swelling, or anaphylaxis) and a side effect (like nausea or dizziness). It just sees a word: "allergy." And it reacts accordingly.Definite vs. Possible Allergy Alerts
Not all alerts are created equal. There are two main types:- Definite allergy alerts - The drug you’re being given contains the exact ingredient you’re listed as allergic to, or it’s in the same class. For example, if you’re allergic to amoxicillin and someone prescribes penicillin, you’ll get a definite alert.
- Possible allergy alerts - These are based on cross-reactivity. Like being warned against taking cefdinir (a cephalosporin) because you have a "penicillin allergy." But here’s the thing: the risk of cross-reactivity between penicillins and later-generation cephalosporins is less than 2%. Most modern EHRs still treat this like a 50-50 gamble.
Severity Levels and Color Codes
EHR systems use color and wording to show how serious the alert is. But these aren’t standardized across systems. Epic uses four levels:- Yellow - Mild reaction (rash, itching)
- Orange - Moderate (swelling, wheezing)
- Red - Severe (low blood pressure, vomiting)
- Black - Life-threatening (anaphylaxis)
Why Alerts Keep Going Off-Even When They Shouldn’t
Here’s the real issue: EHRs are built on broad assumptions. They assume if you’re allergic to one penicillin, you’re allergic to all. They assume if you had a rash from ibuprofen, you’re allergic to every NSAID. They assume a childhood stomachache means lifelong danger. A 2021 NIH study found that 47% of EHR systems don’t even record what kind of reaction the patient had. So if you typed "allergic to penicillin" in 2010, the system still treats it like a death sentence today-even if you’ve taken amoxicillin twice since then without a problem. And it’s not just doctors. Pharmacists get overwhelmed. A 2022 survey by the American Society of Health-System Pharmacists showed 63% of pharmacists say more than half of the allergy alerts they see are irrelevant. One pharmacist in Perth told me: "I’ve seen alerts for azithromycin because someone had a headache after taking it. That’s not an allergy. That’s a headache. But the system doesn’t know that."How to Actually Use These Alerts
You can’t ignore them. But you also can’t trust them blindly. Here’s how to read them right:- Check the reaction description. Was it hives? Swelling? Trouble breathing? Or nausea, diarrhea, dizziness? Only the first three are true allergic reactions.
- Look at the timing. True allergic reactions happen within minutes to hours after taking the drug. If you had a reaction two weeks later, it’s probably not allergic.
- Ask if it was tested. Did a doctor confirm this with a skin test or challenge? Or was it just assumed?
- Know the drug class. Penicillin and cephalosporins? Cross-reactivity is rare. NSAIDs? Most people aren’t truly allergic-they just get stomach upset.
- Ask yourself: Have I taken this before? If you’ve taken azithromycin or cefdinir before without issue, the alert is likely a false alarm.
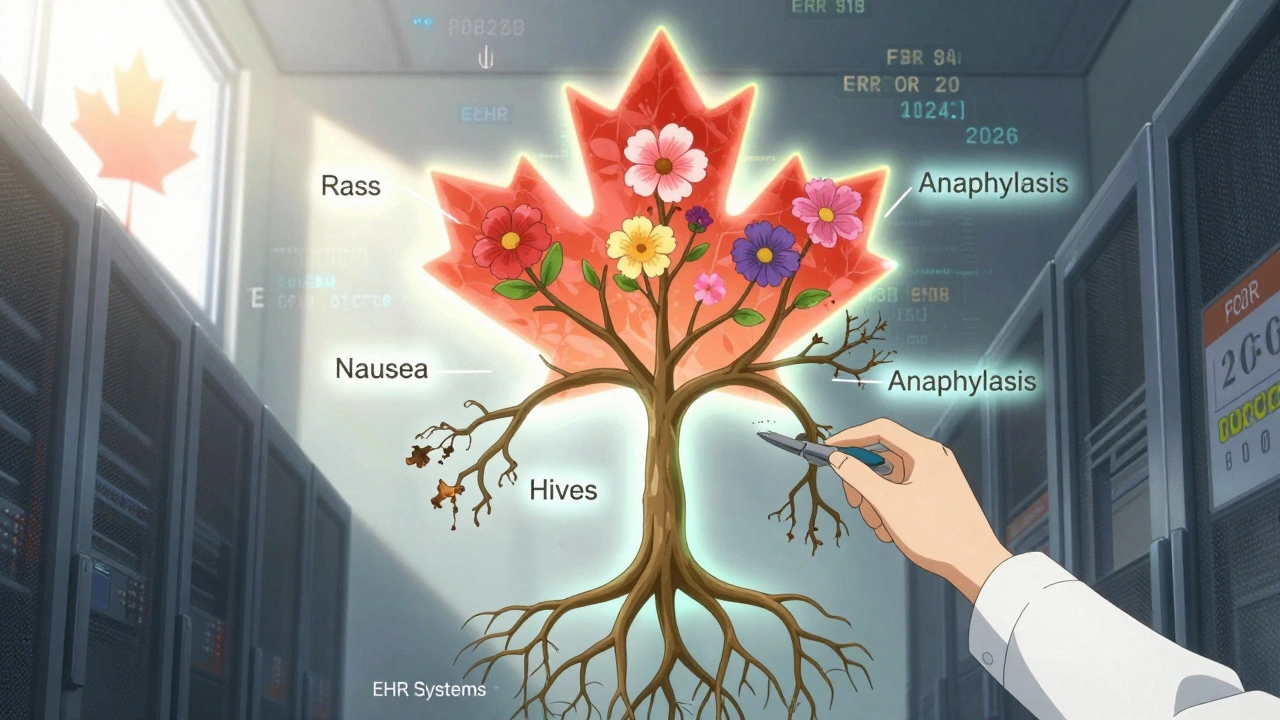
What’s Changing-And What’s Coming
The system is starting to fix itself. Epic’s 2023.2 update introduced "Allergy Relevance Scoring," which uses machine learning to predict which alerts are likely to be false. At Intermountain Healthcare, it cut low-value alerts by 37%. Oracle Health (formerly Cerner) now has a "Precision Allergy" module that pulls in results from allergist testing. If you’ve been tested and cleared of a penicillin allergy, the system auto-removes the alert. The 21st Century Cures Act, effective January 1, 2023, now requires EHRs to use structured documentation. That means instead of typing "allergic to penicillin," you now have to pick from a menu: "anaphylaxis," "hives," "rash," "nausea," "other." This small change is already improving accuracy. By 2026, 70% of major EHR systems are expected to use risk-stratified alerts-where only true, high-risk reactions trigger strong warnings. That means fewer false alarms… and more attention paid to the real dangers.What You Can Do Right Now
You don’t need to wait for the system to improve. Here’s what you can do:- Review your allergy list at every doctor’s visit. If you wrote down "penicillin allergy" because you got sick as a kid, ask: "Was that ever confirmed?"
- Ask for a test if you think you might not be allergic. Penicillin skin tests are safe, quick, and covered by most insurance.
- Update your records if you’ve taken a drug since being labeled "allergic" and had no reaction. Your doctor can remove the alert.
- Carry a list of what you’ve actually reacted to-written clearly. Don’t rely on the pharmacy’s system alone.
What’s the difference between a drug allergy and a side effect?
A drug allergy involves your immune system reacting to a medication-causing symptoms like hives, swelling, trouble breathing, or anaphylaxis. A side effect is a non-immune reaction, like nausea, dizziness, or stomach upset. Most "allergy" alerts are triggered by side effects, not true allergies.
Can I outgrow a drug allergy?
Yes. Many people labeled allergic to penicillin as children lose the sensitivity over time. Studies show that 80% of people who think they’re allergic to penicillin aren’t-even 10 years later. A simple skin test can confirm whether you’re still allergic.
Why do I get allergy alerts for drugs I’ve taken before?
EHR systems don’t track whether you’ve taken a drug since the allergy was recorded. If you had a rash from amoxicillin in 2015 and took it again in 2020 without issue, the system still flags it. That’s why you need to update your allergy list with your doctor.
Are cephalosporins safe if I’m allergic to penicillin?
For most people, yes. The risk of cross-reactivity between penicillin and third- or fourth-generation cephalosporins is less than 2%. Older systems treated all cephalosporins as risky, but newer ones now differentiate by generation. Still, always check with your doctor or pharmacist if you’re unsure.
What should I do if a pharmacist says I’m allergic to a drug I’ve taken safely?
Ask them to check your allergy documentation. If it just says "penicillin allergy" without details, request a review. You can also ask your doctor to update your record and provide a note explaining your history. Many pharmacists will adjust the alert once they have accurate information.


Comments
Heidi Thomas December 5, 2025 AT 15:18
This whole system is a joke. People write 'allergic to penicillin' because they got a stomach ache at 12 and now we're all stuck with overblown alerts that make pharmacists look like robots. I've had 3 prescriptions overridden because of this nonsense. The system doesn't know the difference between a side effect and an allergy and neither do most doctors. Fix the database, not the warnings.
Martyn Stuart December 7, 2025 AT 03:42
Exactly. I'm a pharmacist in rural Maine and 7 out of 10 alerts I see are for things like 'penicillin allergy' with no reaction details. One guy came in for azithromycin because he had a headache after taking amoxicillin in 2008. Headache. Not hives. Not swelling. Just a headache. The system doesn't care. We're drowning in noise. The new Epic scoring update is a start, but we need mandatory fields for reaction type. No more free-text 'allergy' entries.
Ashley Elliott December 9, 2025 AT 02:43
I appreciate you breaking this down. I used to panic every time I saw an alert, but now I just check the reaction type. My mom was labeled allergic to penicillin because she got a rash as a kid-turned out it was a virus. She got tested last year and it was cleared. Took 30 years, but now she can take any beta-lactam without fear. Small wins matter.
Jessica Baydowicz December 9, 2025 AT 02:43
YESSSS this is the kind of info we NEED to be shouting from the rooftops!! 🙌 I used to avoid all antibiotics like they were poison because of a childhood stomachache. Now I know it was just my 8-year-old gut being dramatic. Go get tested if you think you might be mislabeled-you’re not being dramatic, you’re being smart. Your future self will thank you 💪💊
Jordan Wall December 10, 2025 AT 03:30
Of course the system's flawed-EHRs are built by consultants who've never met a patient. It's all about liability, not logic. The real issue? Clinicians are too lazy to dig into the details. They override because they're overworked, not because they're informed. This isn't a tech problem-it's a cultural one. We've outsourced critical thinking to algorithms and now we're paying the price. 🤖
Gareth Storer December 12, 2025 AT 00:28
So what you're saying is... we're all just guinea pigs in a $20 billion software experiment that can't tell the difference between a rash and a sneeze? Brilliant. Just brilliant. Next they'll warn me about aspirin because I once sneezed after taking it. At least my cat doesn't have an EHR. She gets to live in peace.
Pavan Kankala December 13, 2025 AT 01:24
They’re not wrong. It’s not a glitch-it’s a control mechanism. The pharmaceutical industry wants you to believe you’re allergic so they can sell you expensive alternatives. Penicillin is cheap. Cephalosporins? Not so much. The system’s designed to funnel you into branded drugs. Don’t be fooled. Your allergy? Probably a marketing tactic.
Gillian Watson December 14, 2025 AT 10:48
Love this. I’m from London and we’ve got the same mess here. My GP finally updated my record after I showed her my old hospital notes-turns out I had a reaction to a dye, not the antibiotic. Took me 12 years to get it fixed. The system’s broken, but patients can fix it if they’re persistent. Just don’t give up.
Karl Barrett December 14, 2025 AT 14:35
There’s a deeper philosophical layer here: we’ve outsourced our medical memory to machines. We no longer know our own bodies because the system tells us who we are. The allergy alert isn’t just a warning-it’s a narrative imposed on us. Who are we if not the data points we’ve been tagged with? The real crisis isn’t false positives-it’s the erosion of personal medical agency.
Jake Deeds December 14, 2025 AT 16:45
Wow. I just realized I’ve been living under a false allergy label since I was 6. I’ve missed out on life-saving antibiotics because of a 1998 stomach bug. My parents never questioned it. I never questioned it. This isn’t just a system failure-it’s a generational trauma. I’m booking a skin test tomorrow. Thank you for this wake-up call.
val kendra December 15, 2025 AT 00:23
Update your records. Seriously. It takes five minutes. Go to your portal, find your allergies, click edit, and pick the right reaction. If it says 'rash' instead of 'allergy' it changes everything. I did it last year and now my pharmacist actually nods instead of panics. Small step, huge difference. You’re not being difficult-you’re being smart.
Yasmine Hajar December 15, 2025 AT 19:43
My niece had a reaction to amoxicillin-hives, fever, the whole thing. They tested her, confirmed it, and she’s now in the system with a RED alert. But my brother? He had a stomachache at 7 and it got logged as 'penicillin allergy' with no details. He just got prescribed cefdinir for pneumonia and the system screamed like a fire alarm. He had to call his doctor to override it. This isn’t safety-it’s chaos. We need better data, not louder alarms.
Isabelle Bujold December 17, 2025 AT 09:59
As someone who’s worked in pediatric allergy clinics for over 20 years, I can tell you this: 80% of penicillin allergies are mislabeled. Most people outgrow them. Most never had them to begin with. The real danger isn’t the drug-it’s the assumption. We’ve created a culture of fear around antibiotics because we don’t teach patients how to interpret their own records. A simple chart showing immune-mediated reactions vs. side effects should be mandatory in every primary care office. And yes, skin tests are safe, quick, and covered. Stop letting outdated data dictate your health.
Dematteo Lasonya December 17, 2025 AT 16:09
Thank you for writing this. I used to feel guilty for asking my pharmacist to check my records. Now I know I’m not being difficult-I’m being responsible. My daughter’s allergy list was a mess until we sat down with her pediatrician and clarified each entry. We changed 'nausea' to 'side effect' and 'rash' to 'viral exanthem'. It felt like reclaiming her medical identity. This matters. It really does.
Shofner Lehto December 18, 2025 AT 16:22
Just a quick note: if you’re ever told you’re allergic to penicillin, ask for a skin test. It’s painless, takes 20 minutes, and costs less than your co-pay. If you’ve taken it before without issue, you’re probably not allergic. Don’t let a 15-year-old error stop you from getting the right treatment. Your future self will thank you.