Every time you pick up a prescription, the little paper label on the bottle holds life-or-death information. But most people barely glance at it. They see the name of the drug, the dosage, and the number of pills - and that’s it. What they miss? The hidden warnings that could stop a dangerous drug interaction before it starts.
Every year in the U.S., about 2 million adverse drug events happen because people didn’t understand what was on their prescription label. Around 100,000 of those lead to hospital stays. And here’s the scary part: most of them are preventable. The problem isn’t the medicine. It’s the label.
What’s Actually on Your Prescription Label?
The FDA requires every prescription label to follow a strict format. It’s not random. Each section has a purpose, and the most important one for avoiding interactions is right there in plain sight - the Drug Interactions section (Section 7) and the Warnings and Precautions section (Section 5).
These aren’t just filler. They’re legally required to tell you three things: there’s a problem, how bad it is, and what to do about it. That’s the rule as of June 2024. No more vague warnings. If a drug can cause dangerous bleeding when mixed with another, the label has to say so clearly.
Look for phrases like:
- “Avoid concomitant use of [Drug A] with [Drug B]”
- “Reduce dosage of [Drug A] when used with [Drug B]”
- “Monitor for [specific symptom] such as dizziness, bruising, or irregular heartbeat”
These aren’t suggestions. They’re instructions. Ignoring them isn’t risky - it’s reckless.
Don’t Forget Over-the-Counter and Supplements
Most people think prescription drugs are the only danger. But the real hidden threat? The stuff you buy without a prescription.
Over-the-counter painkillers like ibuprofen or naproxen can increase bleeding risk when taken with blood thinners like warfarin. Antacids can make antibiotics useless. Even common cold medicines can raise blood pressure if you’re on heart medication.
And supplements? They’re the silent killers. Ginkgo biloba, garlic pills, St. John’s wort - these aren’t harmless. A 2023 Harvard study found that 147 cases of dangerous bleeding were linked to people taking warfarin and herbal supplements - and not one of those supplements was listed on their prescription label. Why? Because supplement makers aren’t required to warn about drug interactions.
The FDA doesn’t regulate supplements like drugs. That means the label on your vitamin bottle might say “Supports immune health,” but it won’t say “May cause life-threatening bleeding with blood thinners.” You have to know that on your own.
How to Actually Read the Label - Step by Step
Reading a prescription label isn’t about skimming. It’s about hunting for clues. Here’s how to do it right:
- Start with the Warnings section. This is where the FDA requires the most serious interaction alerts. Look for bold text, red flags, or phrases like “contraindicated” or “avoid.”
- Find the Drug Interactions section. This is usually Section 7. It’s longer and more detailed. Don’t skip it because it’s dense. Look for the names of drugs you’re already taking - even if they’re not on this bottle.
- Check the active ingredients. If you’re taking Tylenol for pain and your prescription is also acetaminophen, you’re doubling your dose. That can cause liver damage. Same goes for cold medicines that contain diphenhydramine - if you’re also taking a sleep aid with the same ingredient, you’re overdosing.
- Look for food or alcohol warnings. Some drugs can’t be taken with grapefruit juice. Others can’t be mixed with alcohol. These are easy to miss, but they’re just as dangerous as drug-to-drug interactions.
- Ask yourself: “What’s the bottom line?” The FDA now requires labels to make the key takeaway obvious. If you can’t tell what to do after reading it, you’re not reading it right.
One simple trick? Write down the reason you’re taking each pill. Instead of just “Klonopin,” write “Klonopin - for anxiety.” That stops you from mixing up similar-sounding drugs like clonidine (for blood pressure) and clonazepam (for seizures). That mix-up causes 12% of prescription errors reported to the FDA.
Why You Can’t Rely on Apps Alone
You’ve probably used Drugs.com or WebMD’s interaction checker. They’re helpful. But they’re not enough.
Apps cover about 92% of prescription drugs. That means 8% are missing. Prescription labels cover 100%. Apps don’t know your exact dosage, your kidney function, your age, or whether you’ve had a reaction before. The label does. It’s tied to your specific medication batch and manufacturer’s testing.
Also, apps give you a list of possible interactions. They don’t tell you what to do. The label does: “Reduce dose by 50%,” “Check liver enzymes weekly,” “Stop immediately if rash appears.” That’s the difference between a warning and a plan.
Use apps as a second check - not your first line of defense.
What to Do When You’re Taking Five or More Medications
If you’re on five or more prescriptions, your risk of a dangerous interaction jumps dramatically. A CDC survey found that 68% of people on five or more meds couldn’t identify potential interactions from their labels alone.
Here’s what works:
- Make a complete list. Include every pill, patch, liquid, vitamin, herb, and supplement. Don’t leave anything out. Even if you think it’s “just a vitamin.”
- Bring the list to every doctor and pharmacist. Don’t assume they know what you’re on. A 2023 study of 10,000 pharmacy visits found that 22% of interactions were caught only because the patient brought their full list.
- Ask your pharmacist to review it all. Pharmacists are trained to spot interactions. They see hundreds of these lists every week. Use their expertise.
- Use the “Check the Label” method for kids. If you’re giving medicine to a child, read the label, follow the directions, and use the measuring tool that came with the bottle. Misreading doses causes 67% of pediatric errors.
What’s Changing - And What You Should Know
The FDA just updated its labeling rules in June 2024. New labels will start appearing in pharmacies by Q3 2025. The big changes:
- Critical warnings will be in bold text.
- Each interaction section will start with a clear “bottom line” summary.
- QR codes will appear on some labels, linking to updated, easy-to-read interaction guides.
These changes are coming because the old system failed too many people. A 2023 study found that only 38% of doctors could find the key interaction info in a label within 30 seconds. That’s not acceptable.
But here’s the catch: QR codes and bold text won’t help if you don’t read the label. The technology is improving - but your attention is still the most important tool.
Real Stories, Real Consequences
On Reddit, people share stories every week about how they almost died because they ignored a label.
One woman took ibuprofen with her blood thinner. She didn’t see the warning because it was buried in small print. She ended up in the ER with internal bleeding.
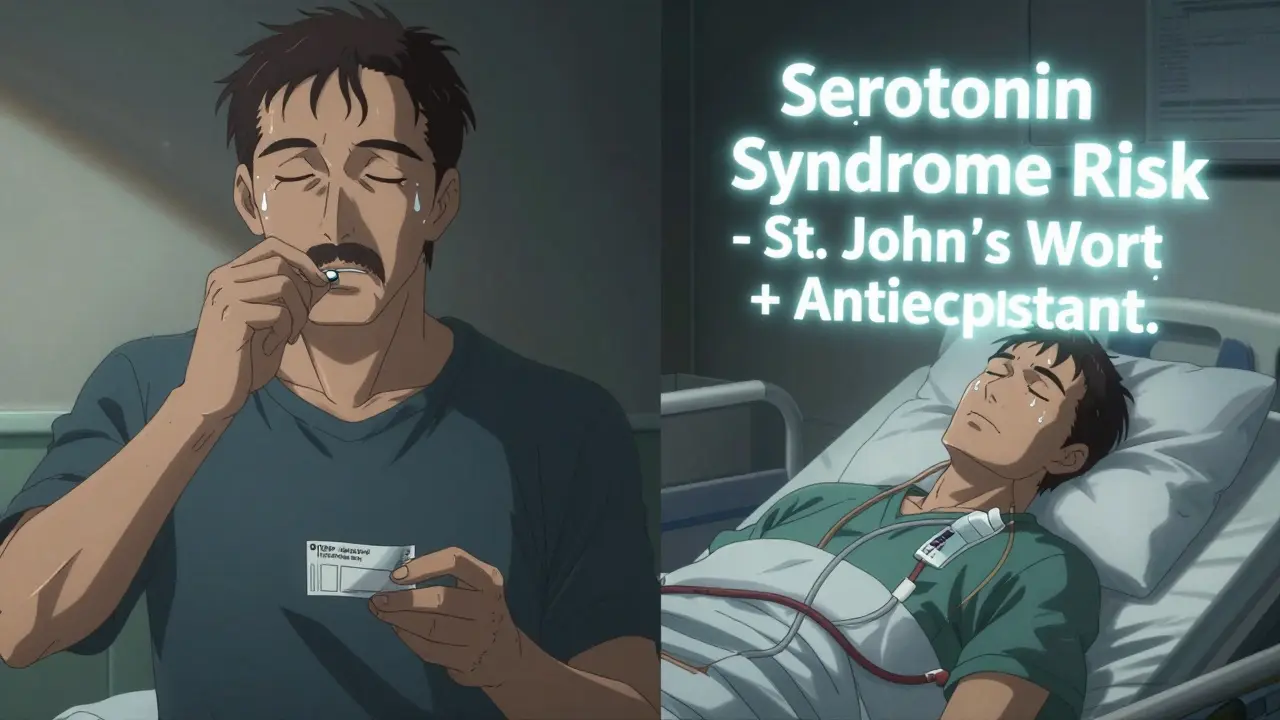
Another man took St. John’s wort for depression while on an antidepressant. He didn’t know it could cause serotonin syndrome - a potentially fatal condition. He was hospitalized for five days.
These aren’t rare. They’re predictable. And they’re preventable.
The bottom line? Your prescription label isn’t junk mail. It’s your safety manual. Treat it like one.
What to Do Next
Here’s your action plan - today:
- Grab every prescription, OTC bottle, and supplement container you’re currently taking.
- Write down the name, dosage, and reason for each one.
- Find the “Drug Interactions” and “Warnings” sections on each label. Highlight anything that says “avoid,” “monitor,” or “reduce.”
- Take that list to your pharmacist and ask: “Are any of these dangerous together?”
- Set a phone reminder to check your labels every time you refill a prescription. Things change. Labels update.
You don’t need to be a doctor to protect yourself. You just need to read the label - and take it seriously.


Comments
Aparna karwande January 8, 2026 AT 01:05
Oh please. You think this is about reading labels? It’s about the pharmaceutical industry deliberately burying warnings in tiny font so you’ll keep buying their poison. I’ve seen labels where the word ‘DEADLY’ is printed in 6pt font while the brand name is in 24pt. This isn’t safety-it’s corporate malice wrapped in bureaucratic legalese. And don’t even get me started on how the FDA is owned by Big Pharma. You think they want you to understand your meds? No. They want you to trust the bottle and shut up.
Jessie Ann Lambrecht January 9, 2026 AT 12:32
This is so important and I’m so glad someone laid it out clearly. I’m a pharmacist and I see people miss life-threatening interactions every single day because they skim. Seriously-take five minutes when you pick up a script. Write down every pill, even that ‘harmless’ ginkgo you got on Amazon. I had a patient last week who mixed St. John’s wort with SSRIs and ended up in ICU. It’s not scary to read the label-it’s scary not to. You’ve got this.
Vince Nairn January 9, 2026 AT 21:50
lol so now we’re supposed to be pharmacists too? next they’ll make us memorize the chemical structure of every pill we take. i mean sure read the label if you want but 90% of people dont even know what 'concomitant' means. the system is broken not the people. just give us a green light or red light app. why make us read 12 paragraphs about bleeding risk when all i want to know is ‘will this kill me’
Kyle King January 10, 2026 AT 03:38
They’re not warning you because they care. They’re warning you because they got sued. Every single ‘dangerous interaction’ on that label was known for decades. The FDA didn’t force this change because people were dying-they did it because a lawsuit made headlines. And don’t you dare trust a QR code. Those are tracking devices. They’re logging what meds you take, who you are, and selling it to insurers. You think they want you to live? They want you to be predictable. Read the label? Nah. Burn it. Don’t let them monitor your body.
Emma Addison Thomas January 11, 2026 AT 04:04
It’s interesting how the American system places so much responsibility on the individual, when in the UK we’re taught from a young age to consult a pharmacist as a first step-not to self-diagnose via label reading. I’ve seen people here stress over tiny print when a simple five-minute chat with the pharmacist would’ve cleared everything up. Perhaps the real issue isn’t the label’s clarity, but the cultural expectation that patients must be their own medical detectives. I admire the intent, but the burden feels misplaced.
Mina Murray January 12, 2026 AT 04:57
Ugh. This is why people die. You think the label is the problem? No. It’s the fact that you’re taking ANY of this crap. Why are you on five meds? Why are you popping St. John’s wort like candy? Why do you trust a doctor who prescribes you a drug that’s been recalled in Europe? The label is the least of your problems. You’re not sick-you’re lazy. And you’re trusting corporations and charlatans to fix your life. Read the label? No. Stop taking everything. Go outside. Eat real food. Sleep. That’s the real interaction you’re missing.
Rachel Steward January 12, 2026 AT 23:24
Let’s be brutally honest: the entire pharmacological model is a performative illusion of control. The label is a theater prop-designed to absolve the system of moral responsibility while making you feel like you’re in charge. You read the warning, you feel virtuous, you check the box. But you’re still a cog. You don’t know why you’re taking the drug. You don’t know the clinical trial data. You don’t know the manufacturer’s profit margins. The label doesn’t tell you the truth-it tells you what they want you to believe is the truth. You think ‘avoid concomitant use’ means safety? No. It means liability. The label is a legal shield, not a lifeline. And you? You’re the shield’s target.
Jonathan Larson January 13, 2026 AT 13:25
While the sentiment of vigilance is commendable, one must acknowledge the broader structural context. The onus of medical literacy should not rest solely upon the layperson, particularly when systemic barriers-including time constraints, language accessibility, and socioeconomic disparities-impede comprehension. A well-designed label is necessary but insufficient. True progress requires integration of patient education into primary care, pharmacist-led counseling as a standard of care, and regulatory enforcement that prioritizes clarity over compliance. The label is a tool; it is not the solution.
Katrina Morris January 15, 2026 AT 11:42
I just checked my meds and found I’ve been taking two things with the same active ingrediant and didn’t even know it. I’m so glad I read this. I’m gonna take my list to the pharmacy tomorrow. Thanks for the nudge.