If you’re struggling to afford your prescription, you’re not alone. Nearly 1 in 3 Americans skip doses or don’t fill prescriptions because of cost. But there’s a proven way to cut your medication expenses without sacrificing effectiveness: asking for a therapeutic alternative. This isn’t about switching to a generic version of the same drug. It’s about swapping your current medication for a different one that works just as well-often for a fraction of the price.
What Is a Therapeutic Alternative?
A therapeutic alternative is a different drug that treats the same condition as your current prescription, but belongs to a different chemical class or is a different brand. For example, if you’re taking esomeprazole (Nexium) for acid reflux, your doctor might suggest switching to omeprazole. Both are proton pump inhibitors. Both reduce stomach acid. But omeprazole costs about $15 a month as a generic, while Nexium can run over $300. That’s a 95% savings. This isn’t a loophole. It’s a standard medical practice backed by decades of clinical research. Studies show that for conditions like high blood pressure, diabetes, and depression, therapeutic alternatives often deliver the same results as brand-name drugs-with fewer financial headaches.Why Most People Don’t Ask
Many patients assume their doctor already knows the cheapest option. Or they worry their doctor will think they’re being cheap. Others don’t know where to start. But here’s the truth: doctors want you to take your meds. They’re not trying to make you spend more. If you bring up cost, they’re legally and ethically obligated to help. A 2023 survey by the American Academy of Family Physicians found that 78% of primary care doctors regularly consider therapeutic alternatives-but only if the patient brings it up. You have to start the conversation.How to Ask for a Lower-Cost Alternative
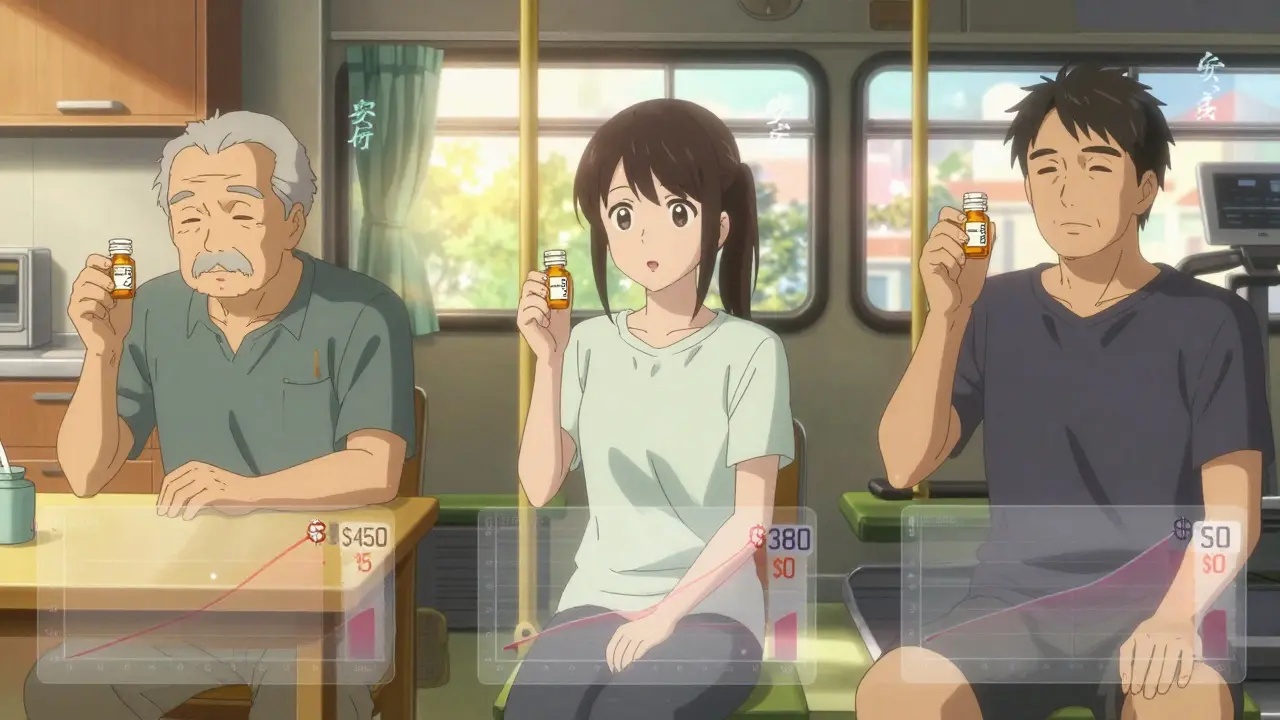
Here’s exactly how to do it-step by step.- Check your current medication’s cost. Use GoodRx or similar tools to compare prices at local pharmacies. You might be surprised. One patient found that their $450 monthly Lyrica prescription dropped to $15 with gabapentin, a therapeutic alternative. That’s not a typo.
- Do a quick search. Look up your drug and the phrase “therapeutic alternative.” You’ll find lists from trusted sources like Healthgrades, NeedyMeds, and the Institute for Clinical Systems Improvement. For example, if you’re on Eliquis (apixaban) for blood clots, warfarin is a proven alternative that costs under $10 a month.
- Prepare your ask. Don’t say, “This is too expensive.” Say, “I’m having trouble affording this. Are there other medications that work just as well but cost less?” Be specific. “Could I try omeprazole instead of esomeprazole?”
- Bring data. Print or show your doctor the cost difference. Mention that studies show these switches work. For instance, a 2017 Vanderbilt study found no drop in effectiveness when patients switched from brand-name drugs to therapeutic alternatives.
- Ask about extended prescriptions. Even if you can’t switch drugs, getting a 90-day supply instead of 30 can cut your copay by up to 25%. Many insurers charge the same for a 90-day supply as they do for 30 days.
When It Works Best
Therapeutic alternatives shine in chronic conditions where you take medication daily for months or years. Think:- High blood pressure: lisinopril instead of benazepril
- Diabetes: metformin instead of Jardiance
- Cholesterol: atorvastatin instead of Crestor
- Depression: sertraline instead of escitalopram
- Acid reflux: famotidine instead of ranitidine (though ranitidine is now off the market, famotidine is still widely used)
When It Doesn’t Work
Not every drug has a safe alternative. This is especially true for:- Biologics used in autoimmune diseases (like Humira or Enbrel)
- Cancer treatments
- Some rare neurological conditions
What to Do If Your Doctor Says No
Sometimes, doctors hesitate because they’re unfamiliar with alternatives or worry about side effects. That’s normal. But you can push back-politely.- Ask: “Is this because of safety, or just habit?”
- Offer to try it under supervision: “Could we try the alternative for 30 days and check in?”
- Request a tiering exception with your insurance. If your plan denies coverage for your current drug, you can ask for an exception based on cost. Medicare Part D requires a decision within 72 hours for urgent cases.
Real Savings, Real Stories
- A 68-year-old man switched from Eliquis to warfarin. His monthly cost dropped from $450 to $12. He now takes his meds every day. - A woman with type 2 diabetes switched from Jardiance to metformin. Her copay went from $85 to $5. Her blood sugar stayed stable. - A man on brand-name Crestor switched to atorvastatin. He saved $380 a month. He started going to the gym again because he wasn’t stressed about money anymore. These aren’t outliers. GoodRx’s 2024 survey of 12,500 patients found that 68% successfully got a lower-cost alternative. The average monthly savings? $47.25. That’s over $560 a year.
Tools to Help You
You don’t need to guess. Use these free resources:- GoodRx - Compares prices across 70,000+ pharmacies. Shows therapeutic alternatives.
- NeedyMeds - Lists patient assistance programs, copay cards, and discount coupons.
- RxAssist - Free database of drug savings programs from drugmakers.
- Healthgrades’ $4 Generic List - Lists common meds like metformin, lisinopril, and atorvastatin available for $4 at Walmart, CVS, and Walgreens.
What to Watch Out For
Not all alternatives are safe for everyone. A 2024 JAMA case report described a patient who switched from Taltz (a biologic for psoriasis) to methotrexate. Their condition worsened, leading to $18,000 in emergency care. That’s why you never self-switch. Always consult your doctor. Even if the alternative is cheaper, it must match your health profile. If you have kidney disease, for example, some blood pressure drugs are riskier than others. Also, don’t assume insurance covers the alternative. Some plans still require prior authorization-even for generics. Ask your pharmacist to check your coverage before you fill the script.Final Thought: You Have Power
Medication costs aren’t set in stone. They’re negotiable. You’re not asking for a favor-you’re exercising your right to affordable care. Therapeutic interchange isn’t a last resort. It’s a smart, evidence-based strategy that doctors are trained to use. Start with one medication. Use GoodRx to check the price. Write down your question. Bring it to your next appointment. You might save hundreds-or even thousands-without changing how you feel.Can I switch to a therapeutic alternative without my doctor’s approval?
No. Even if a medication is cheaper, you should never switch on your own. Different drugs have different side effects, dosing schedules, and interactions. What works for one person may not work for another. Always talk to your doctor or pharmacist before making any change.
Are therapeutic alternatives as effective as brand-name drugs?
Yes, when chosen correctly. Clinical trials have shown that many therapeutic alternatives produce identical outcomes for conditions like high blood pressure, depression, and acid reflux. For example, a 2017 study from Vanderbilt University found no difference in patient outcomes when switching from brand-name drugs to therapeutic alternatives. The key is matching the drug to your condition and medical history.
Why do some doctors resist therapeutic alternatives?
Some doctors aren’t familiar with the latest cost data or worry about patient safety. Others assume brand-name drugs are superior, even when evidence shows otherwise. A 2023 survey found that 43% of patients faced initial resistance from providers. Bringing printed data or using phrases like “I found a study showing this works just as well” can help overcome this.
Does Medicare cover therapeutic alternatives?
Yes, and Medicare Part D plans are required to cover them. If your current drug is on a higher tier, you can request a tiering exception based on cost. As of 2025, CMS mandates that these requests be processed within 72 hours for urgent cases. Many therapeutic alternatives are on the lowest cost tier, so you may not even need an exception.
How much can I realistically save?
It varies, but most patients save between $30 and $400 per month. For common drugs like atorvastatin, metformin, or lisinopril, savings can be as high as 95%. One patient saved $450 monthly by switching from Eliquis to warfarin. Even smaller savings add up: $10 a month is $120 a year-enough to cover a dental visit or prescription co-pay for another medication.
What if I can’t afford even the alternative?
Many drug manufacturers offer free or deeply discounted programs for low-income patients. NeedyMeds and RxAssist list these for free. You can also apply for state pharmaceutical assistance programs. In Australia, the PBS (Pharmaceutical Benefits Scheme) caps prescription costs at $32.90 for concession card holders and $10.30 for those with a concession card. In the U.S., programs like the HealthWell Foundation help cover copays for over 1,200 medications.
Can I use GoodRx with my insurance?
Sometimes. GoodRx is not insurance. It’s a discount coupon. If the GoodRx price is lower than your insurance copay, you can choose to use GoodRx instead. But you can’t combine them. Always compare the GoodRx price with your insurance price before paying at the pharmacy.
Are there risks with switching to a therapeutic alternative?
There can be, if the switch isn’t managed properly. Some patients may experience side effects or reduced effectiveness, especially with complex conditions like epilepsy or autoimmune disorders. That’s why it’s essential to work with your doctor. Most therapeutic alternatives are safe, but they need monitoring. Ask your doctor to schedule a follow-up in 2-4 weeks after the switch.

Comments
Bryan Wolfe January 10, 2026 AT 14:10
Just switched my dad from Nexium to omeprazole last month-saved him $280 a month, and his heartburn is actually better now. I didn’t believe it either until I saw the receipt. Doctors don’t always bring this up, but they’ll help if you ask. Seriously, just say it: ‘Can we try something cheaper?’ It’s not rude, it’s smart.
Prachi Chauhan January 11, 2026 AT 10:48
in india we have this thing called ‘generic medicine’-like, you walk into any pharmacy and ask for ‘metformin’ instead of ‘Jardiance’ and they hand you a packet for 20 rupees. no one bats an eye. here in the us, it feels like you’re asking for a miracle. why is cost so taboo? it’s medicine, not luxury perfume.
Katherine Carlock January 12, 2026 AT 08:51
I literally cried when my pharmacist told me gabapentin was $12 instead of Lyrica’s $450. I’ve been taking it for 3 years and my nerve pain hasn’t gotten worse. My doctor was skeptical at first, but when I showed him the JAMA study? He said ‘you’re right, we should’ve done this sooner.’ I wish I’d known this 5 years ago. You’re not being cheap-you’re being responsible.
Sona Chandra January 13, 2026 AT 07:12
THIS IS WHY AMERICA IS BROKE. DOCTORS AREN’T THE PROBLEM-THEY’RE JUST FOLLOWING THE PHARMA PLAYBOOK. BIG PHARMA MAKES BILLIONS OFF BRAND NAMES AND THE SYSTEM IS DESIGNED TO KEEP YOU PAYING. I SAW A WOMAN ON TV LAST WEEK WHO HAD TO CHOOSE BETWEEN HER MEDS AND HER KIDS’ SCHOOL SUPPLIES. THIS IS CRIMINAL. AND NO ONE’S DOING ANYTHING ABOUT IT.
Jennifer Phelps January 14, 2026 AT 05:26
so i tried asking my doc about atorvastatin instead of crestor and he just said ‘we’ll stick with what works’ and didn’t even look at the cost difference. i printed out the goodrx prices and he still didn’t budge. i just paid out of pocket for 2 months and now i’m on the cheaper one. no one helped me. i had to fight for it.
beth cordell January 15, 2026 AT 08:37
OMG YES!! 🙌 I switched from Eliquis to warfarin last year and now I can afford to go to the dentist without crying 😭 My pharmacist even gave me a free blood pressure monitor because she said ‘you’re doing everything right.’ You’re not asking for charity-you’re asking for common sense. 💪💊
Lauren Warner January 16, 2026 AT 02:26
Let’s be real. Most of these ‘therapeutic alternatives’ are just old drugs that big pharma stopped marketing. They’re not ‘just as effective’-they’re the ones that haven’t been tested for 15 years. You think your doctor doesn’t know this? They’re just too scared to admit the system is rigged. Don’t trust these ‘savings’-you’re playing Russian roulette with your health.
Craig Wright January 16, 2026 AT 04:29
As a British citizen, I find this entire discussion rather baffling. In the UK, the NHS ensures that all essential medications are available at a flat rate of £9.65 per prescription. If you cannot afford it, you are exempt. The idea that one must negotiate with one’s physician over the cost of a life-saving drug is not merely absurd-it is deeply unseemly. America’s healthcare system remains a moral failure.
Lelia Battle January 17, 2026 AT 16:53
I’ve been thinking about this a lot lately-not just the cost, but the emotional weight of having to ask. It’s not just about money. It’s about dignity. You’re not just negotiating a price-you’re negotiating your right to be healthy. And the fact that you have to fight for that… it’s exhausting. But you’re right to do it. Keep asking. Keep showing up. Your life matters more than the profit margin.
Cassie Widders January 19, 2026 AT 03:31
my mum’s on metformin now. used to be $80, now $4. she didn’t even tell me until she showed me the receipt. said ‘why make you worry?’ i just hugged her. sometimes the quiet wins are the biggest ones.
Alex Fortwengler January 21, 2026 AT 03:27
you think this is new? this is how it’s always been. doctors get kickbacks from pharma reps. they push brand names because they get free lunches and pens with logos. you think they care if you go bankrupt? no. they care if you sign the consent form. this whole ‘therapeutic alternative’ thing is just a PR stunt to make you feel better while they keep raking in cash.
Abner San Diego January 23, 2026 AT 02:03
lol imagine being this excited about switching from one pill to another. you think you’re some kind of healthcare warrior? you’re just a guy who Googled ‘cheaper meds’ and now thinks you’re a doctor. i’ve been on the same med for 10 years. it works. why fix what ain’t broke? also, warfarin? you need blood tests every week. you’re trading money for misery.
steve ker January 23, 2026 AT 12:37
generic is cheaper because it's generic. not because it's better. you think your body doesn't notice the difference? you're a lab rat for big pharma's leftovers. stop pretending you're saving money. you're just accepting lower quality. and don't bring up India. their healthcare is a joke.