Transferring a prescription might seem like a simple task-just call the pharmacy, ask them to move your meds, and you’re done. But if you’ve ever waited days because your new pharmacy couldn’t fill your painkiller, or got a label that said "1.0 mg" instead of "1 mg", you know it’s anything but simple. Prescription transfers aren’t just about moving data from one computer to another. They’re a high-stakes step in keeping you safe from dangerous dosing mistakes, wrong medications, or even life-threatening delays. And the rules around them? They’ve changed a lot recently.
Why Prescription Label Accuracy Matters More Than You Think
Every year in the U.S., about 1.5 million adverse drug events happen because of confusing or incorrect prescription labels. That’s not a guess-it’s from the FDA. These aren’t just inconveniences. They lead to hospital visits, missed work, and sometimes death. One of the most common errors? Trailing zeros. If a label says "5.0 mg", someone might read it as "50 mg". That’s a tenfold overdose. The FDA banned this practice in 2023 after reviewing 327 documented cases between 2018 and 2022. Now, all prescriptions must say "5 mg", not "5.0 mg". Leading zeros matter too. ".4 mg" is a no-go. It has to be "0.4 mg". These tiny details stop people from accidentally taking ten times too much.
Another big issue? Abbreviations. Prescribers used to write "HCTZ" for hydrochlorothiazide or "MOM" for magnesium oxide mixture. But patients don’t know those codes. Pharmacists can’t always guess them correctly. The FDA now recommends writing out the full drug name every time. Same goes for directions. Instead of "q.d.", it should say "once daily". Clear language saves lives.
How Prescription Transfers Work Now-After the 2023 DEA Rule
In August 2023, the Drug Enforcement Administration (DEA) made the biggest change to prescription transfers in over a decade. Before that, you couldn’t transfer a Schedule II prescription-like oxycodone or fentanyl-between pharmacies at all. If you moved, you had to get a new prescription from your doctor. That meant delays. Maybe you went without pain relief for days. Maybe you went to the ER because you couldn’t get your meds.
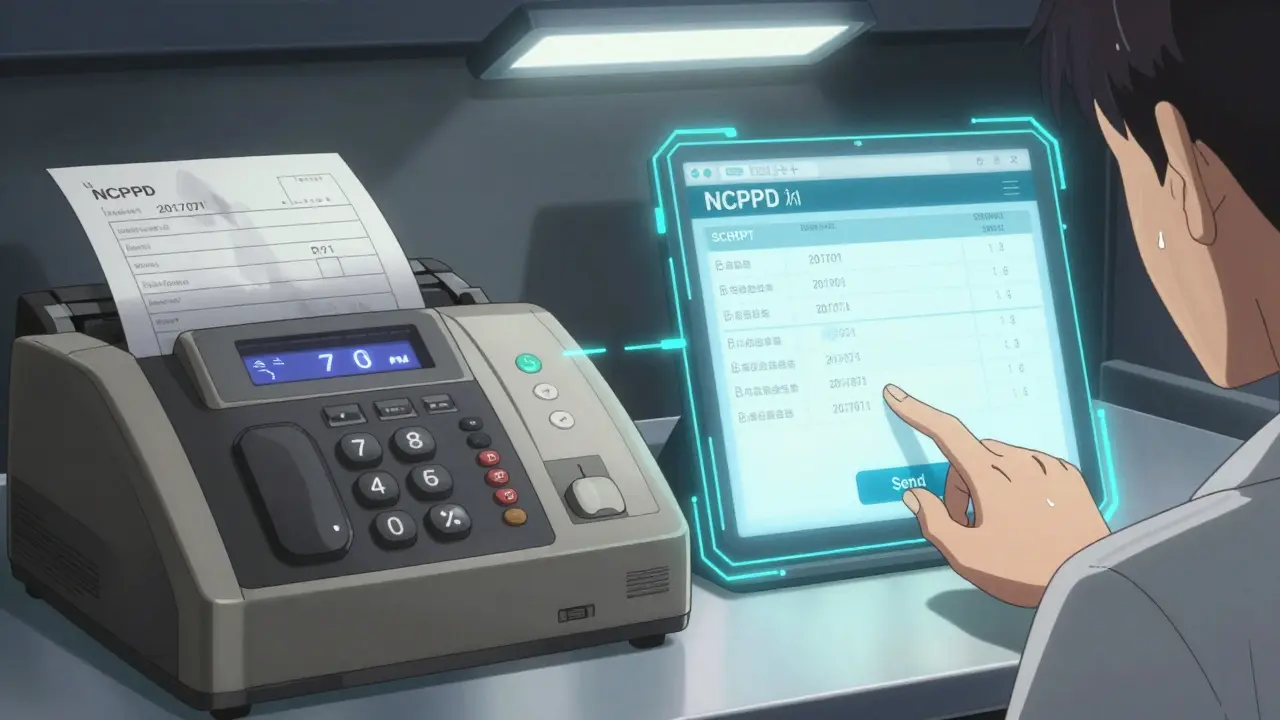
Now, you can transfer Schedule II prescriptions electronically, but only once. That’s it. No second transfer. No fax. No phone call. It has to be a direct electronic transfer between pharmacies using the NCPDP SCRIPT 2017071 standard. And every single piece of data must stay intact. No trimming. No changing. No deleting. If the original says "30 tablets, 10 mg, 3 refills", the new label must show exactly that. Even the date the original was written. Even the name of the pharmacist who filled it the first time.
For Schedule III-V drugs-like codeine cough syrup or anabolic steroids-you can transfer multiple times, up to the number of refills left. Non-controlled drugs? Most states allow unlimited transfers. But the rules still apply: full data, no shortcuts.
What Must Be on Every Prescription Label
The DEA and FDA agree on one thing: every label must have the same core information. Missing one thing? It’s invalid. Here’s what’s required:
- Patient’s full name
- Drug name (written out, no abbreviations)
- Strength (in metric units, no trailing zeros, leading zero if under 1)
- Dosage form (tablet, capsule, liquid, etc.)
- Quantity (how many pills or mL)
- Directions for use (e.g., "Take one tablet by mouth twice daily")
- Prescriber’s full name
- Prescription number
- Date issued
- Number of refills allowed
- Pharmacy name, address, and phone number
That’s it. No extra fluff. No marketing slogans. No "For pain relief only!" on the bottom. Just clear, complete, accurate facts. And if you’re transferring a controlled substance, the pharmacy must also record: the date of the transfer, the name of the pharmacist who sent it, the name of the pharmacist who received it, and the DEA number of the receiving pharmacy. All of this goes into the electronic record.
What Happens If the Systems Don’t Talk?
Not all pharmacies use the same software. Some are on older systems. Some are in rural areas with slow internet. That’s where problems start. In 2022, 18% of pharmacies reported that data got cut off during transfers-sometimes the refill count disappeared, or the directions were truncated. Patients showed up to pick up their meds and got a bottle with no instructions. Or worse: the label said "Take 1 tablet" but the system recorded "Take 10 tablets."
Electronic transfers using the NCPDP SCRIPT standard fix this. A 2022 University of Florida study found they’re 98.7% accurate. Fax? Only 82.3%. Phone? Just 76.1%. That’s why the DEA now requires electronic transfers for Schedule II drugs. But here’s the catch: if the receiving pharmacy’s system can’t accept the data, the transfer fails. And you’re left without meds.
Your Role in Making Transfers Safe
You’re not just a passive passenger in this process. You have to be the quarterback. Before you ask your old pharmacy to transfer your prescription, call the new one. Ask: "Can you accept electronic transfers? Do you have my drug in stock? Can you handle controlled substances?" Don’t assume. Don’t hope. Confirm.
California saw a spike in failed transfers after it allowed outsourcing facilities to fill prescriptions in 2022. Why? 23% of patients didn’t check if the pharmacy could even handle their prescription. One man transferred his oxycodone to a pharmacy that didn’t carry it. He went three days without pain relief. Another woman transferred her insulin-only to find out the new pharmacy didn’t stock the exact brand. She had to drive 40 miles to get it.
And here’s a pro tip: always check the label when you pick it up. Compare it to the old one. Does the strength match? Are the directions the same? If something looks off, say something. Pharmacists are trained to catch errors-but they can’t catch what they never see.

What’s Coming Next: The 2025 Patient Medication Information Rule
The FDA isn’t done. By 2025, every prescription label in the U.S. will have to follow the new Patient Medication Information (PMI) rule. That means:
- Paper labels become the default. Electronic copies are only sent if you ask for them.
- All labels will be scanned by automated systems before they leave the pharmacy.
- Barcode checks will verify drug name, dose, quantity, and patient name.
- Text layout will be standardized-no tiny fonts, no crowded lines.
Early adopters say this reduces errors by up to 40%. But it costs money. In California, pharmacies spent between $12,500 and $18,750 per location to upgrade systems. Independent pharmacies are struggling. Chain pharmacies? 87% are already compliant. Rural pharmacies? Only 41% have the tech.
Bottom Line: Don’t Skip the Verification Step
Transferring a prescription isn’t a formality. It’s a safety checkpoint. Whether you’re moving, changing pharmacies, or just trying to get your meds faster, you need to treat it like a medical procedure. Double-check the label. Confirm the pharmacy can handle it. Ask questions. If you’re on a controlled substance, remember: you only get one shot at a transfer. Get it right the first time.
And if you’re a pharmacist? Don’t cut corners. Use barcode scanners. Verify twice. Record everything. Because in this system, one typo, one missing zero, one unconfirmed transfer-it’s not just a mistake. It’s a risk to someone’s life.
Can I transfer a Schedule II prescription more than once?
No. As of August 2023, the DEA allows only one electronic transfer for Schedule II controlled substances like oxycodone or fentanyl. After that, you must get a new prescription from your prescriber. This rule was put in place to prevent misuse and ensure tight control over high-risk medications.
Why can’t I fax my prescription transfer anymore?
For Schedule II drugs, fax transfers are no longer allowed under the 2023 DEA rule. Only direct electronic transfers using the NCPDP SCRIPT standard are permitted. This is because fax transfers have a 17.7% error rate compared to 1.3% for electronic transfers. The DEA requires full, unaltered data to prevent dosing errors and fraud.
What happens if my label says "1.0 mg"?
That’s a violation of FDA labeling rules. Labels must show whole numbers without trailing zeros-so "1.0 mg" becomes "1 mg." This rule was created because patients and pharmacists have misread "1.0 mg" as "10 mg," leading to dangerous overdoses. Pharmacies are required to correct this before dispensing.
Can I transfer a prescription between states?
Yes, but only if both pharmacies use electronic systems that comply with the DEA’s 2023 rule. State laws still apply, so some states may have extra requirements-like recording the receiving pharmacist’s name on the back of the old prescription. Always check with both pharmacies before initiating the transfer.
How do I know if my new pharmacy can handle my controlled substance?
Call them directly. Ask: "Do you have this medication in stock?" and "Can you accept electronic transfers of Schedule II prescriptions?" Some pharmacies, especially smaller or rural ones, may not carry certain controlled substances or may lack the software to receive them. Don’t assume-confirm before you transfer.


Comments
Larry Zerpa February 21, 2026 AT 21:22
So let me get this straight - you’re telling me I can’t just call my pharmacy and have them fax over my oxycodone anymore? That’s not safety, that’s bureaucracy with a side of suffering. I had to go without pain meds for 72 hours because the new pharmacy ‘couldn’t process the transfer.’ Guess what? I didn’t die. But my quality of life? Gone. This rule feels like it was written by someone who’s never had a chronic condition.