It’s easy to assume that if you break out in hives or feel sick after eating something or taking a pill, it’s an allergy. But not all reactions are allergies-and mixing up food and medication allergies can put your health at risk. One person avoids penicillin for life because they got a rash after taking it as a kid, only to find out decades later it was a virus, not the drug. Another thinks they’re allergic to peanuts because they get stomach cramps after eating them, but it’s actually a food intolerance. These mistakes happen more often than you think. And they’re dangerous.
How Your Body Reacts Differently
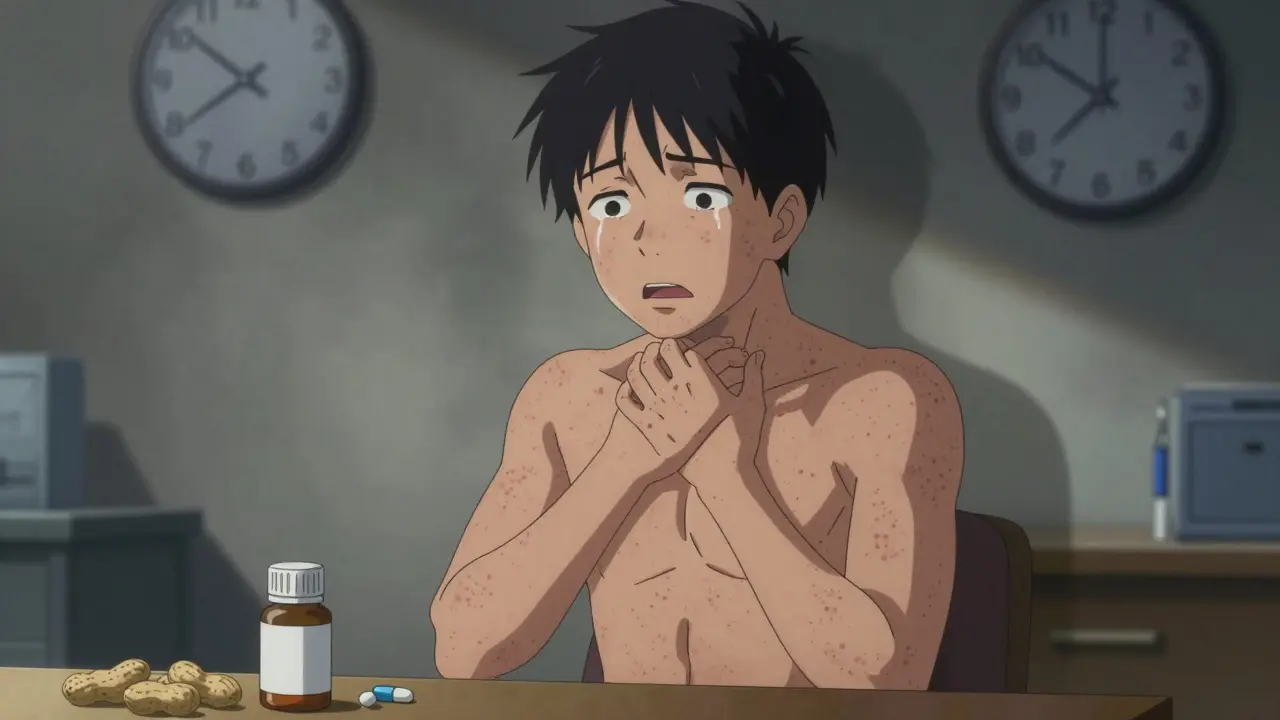
Food allergies and medication allergies both involve your immune system overreacting, but they trigger different pathways. About 90% of food allergies are IgE-mediated. That means your body produces a specific antibody called immunoglobulin E when it sees the allergen-like peanut protein or milk casein. This triggers mast cells to release histamine and other chemicals, causing symptoms within minutes. You might feel your lips tingle, your throat swell, or your skin break out in hives. In severe cases, your blood pressure drops and you struggle to breathe. That’s anaphylaxis, and it can kill. Medication allergies can also be IgE-mediated, but they’re more complex. About 80% of immediate reactions (within an hour) work the same way: think hives or swelling after penicillin. But the other 20% are T-cell mediated, meaning your immune system takes days to react. That’s why you might take amoxicillin for a sinus infection, feel fine for three days, then wake up with a full-body rash, fever, and swollen lymph nodes. That’s DRESS syndrome-a serious delayed reaction. It’s not an allergy in the classic sense, but your immune system is still attacking the drug.When Symptoms Show Up Matters
Timing is one of the clearest ways to tell them apart. With food allergies, 95% of reactions happen within two hours. Most hit within 20 minutes. If you eat shrimp and your tongue swells at 7:15 p.m., it’s almost certainly the shrimp. If you ate the same thing last week and felt fine, it’s not the food. Medication reactions? They don’t follow that rule. Immediate reactions (like hives or wheezing after an IV antibiotic) happen within an hour. But delayed reactions can show up 48 to 72 hours later-or even weeks. A rash from sulfa drugs might not appear until day five. That’s why people often blame the wrong thing. They take a new pill, get sick three days later, and assume the pill caused it. But maybe they also ate sushi that day, or got a cold virus. Without tracking timing precisely, you’re guessing.What Symptoms You Get
Food allergies usually hit the mouth, skin, and gut first. Oral allergy syndrome-itching or swelling in the lips, tongue, or throat-is common with raw fruits and nuts. Vomiting and diarrhea happen in over half of pediatric food allergy cases. Hives appear in nearly 90% of reactions. Respiratory symptoms like wheezing are less common unless it’s a severe reaction. Medication allergies often show up as skin rashes, especially with antibiotics. Maculopapular rashes (flat red spots with bumps) are the hallmark of delayed reactions. Hives can happen too, but they’re less specific. What sets medication reactions apart is how often they cause systemic symptoms: fever, joint pain, swollen glands, or even organ inflammation. These aren’t typical in food allergies unless it’s a life-threatening anaphylactic event. Also, food allergies rarely cause fever. If you get a fever after eating, it’s more likely a virus or food poisoning-not an allergy.Diagnosis Isn’t the Same
For food allergies, skin prick tests and blood tests for IgE antibodies are reliable. But they’re not perfect. A positive test doesn’t always mean you’ll react when you eat the food. That’s why an oral food challenge-eating small amounts under medical supervision-is still the gold standard. It’s safe, controlled, and gives you a definitive answer. Medication allergy testing is trickier. For penicillin, skin testing followed by an oral challenge is 99% accurate at ruling out true allergy. But for most other drugs-like NSAIDs, chemotherapy, or anticonvulsants-there’s no reliable blood or skin test. Doctors have to rely on your history and sometimes do a controlled drug provocation test, where you’re given a tiny dose in a hospital setting. This isn’t done lightly. For drugs like chemotherapy, the risk is too high. So many people are labeled allergic based on a vague history. And here’s the scary part: up to 90% of people who say they’re allergic to penicillin aren’t. They had a rash as a child, or their mom said they were allergic, or they got sick after taking it and never got tested. Yet they’re given stronger, more expensive antibiotics that increase their risk of C. diff infections by 25%.Why Getting It Right Matters
Misdiagnosing a food allergy can be deadly. In the U.S., 150 to 200 people die each year from food-induced anaphylaxis. Most of those deaths happen because symptoms were ignored or mistaken for indigestion. People wait too long to use their epinephrine auto-injector. They don’t realize it’s not just a stomach bug. Misdiagnosing a medication allergy has different consequences. It leads to unnecessary avoidance of safe, effective drugs. People with false penicillin allergies end up on vancomycin or fluoroquinolones-drugs that cost 30% more and are linked to higher rates of antibiotic resistance. Hospitals that run antibiotic delabeling programs-testing patients who claim to be allergic-cut broad-spectrum antibiotic use by 25% and reduce hospital stays. And it’s not just about cost. It’s about care. If you’re labeled allergic to all NSAIDs because you got a rash from aspirin, you might miss out on effective pain relief during surgery or chronic arthritis. You might end up with opioids instead-risking addiction.What You Can Do
If you think you have an allergy, start keeping a detailed log. For food: write down exactly what you ate, how it was prepared, and when symptoms started-down to the minute. Include brand names if possible. Did you eat peanut butter from Brand A or Brand B? Was it roasted or raw? That matters. For medications: record the drug name, dose, time taken, and when symptoms appeared. Did you take it with food? Did you have a fever or virus at the same time? Many rashes from antibiotics are actually caused by viruses, not the drug. But without context, doctors assume the worst. Don’t assume your childhood allergy still applies. About 80% of kids outgrow milk and egg allergies by age 5. Many outgrow wheat and soy allergies by adolescence. But penicillin allergies? They rarely go away on their own. That’s why testing is so important-even if you haven’t taken the drug in 20 years. Ask your doctor for a referral to an allergist. Don’t rely on online quizzes or anecdotal advice from forums. Real testing is the only way to know for sure. And if you’ve been told you’re allergic to a drug, ask: “Has this been confirmed with testing?” If not, it might be time to get checked.
Common Misconceptions
You don’t have to avoid every food or drug if you’re allergic to one. Just because you’re allergic to peanuts doesn’t mean you’re allergic to all nuts. Tree nuts and peanuts are different. Just because you reacted to amoxicillin doesn’t mean you’re allergic to all penicillins-or even all antibiotics. Also, intolerance isn’t allergy. Lactose intolerance causes bloating and diarrhea because you lack the enzyme to digest milk sugar. It’s not an immune response. Same with gluten sensitivity-most people who think they’re allergic to gluten are actually reacting to FODMAPs, not gluten proteins. Allergies involve the immune system. Intolerances don’t. And don’t confuse side effects with allergies. Nausea from antibiotics? That’s a side effect. A rash? That could be an allergy. Headache after ibuprofen? Common side effect. Swelling of the face? That’s a red flag.What’s New in Testing
In 2023, the FDA approved a new blood test called ImmunoCAP® Penicillin that can distinguish true penicillin allergy from false positives with 98% accuracy. For food allergies, component-resolved diagnostics (CRD) now let doctors test for specific proteins in foods. For example, if you test positive for Ara h 2 in peanuts, you’re at high risk for anaphylaxis. If you test positive for Ara h 8, you likely have pollen-food syndrome-your reaction is mild and tied to seasonal allergies. These tools are changing how we diagnose. But they’re not everywhere. Many clinics still rely on old methods. That’s why it’s up to you to ask the right questions.Can you outgrow a food allergy?
Yes, many children outgrow allergies to milk, eggs, wheat, and soy-about 80% by age 5. Peanut, tree nut, fish, and shellfish allergies are less likely to be outgrown, but some people do. Testing every few years under medical supervision can confirm if the allergy has resolved.
Can you develop a medication allergy later in life?
Absolutely. Medication allergies can appear at any age. The average age of first reaction is 42. You might take penicillin safely for years, then suddenly develop hives after a course of amoxicillin. This happens because your immune system changes over time. Never assume past tolerance means future safety.
Is a rash always a sign of a drug allergy?
No. Many rashes that appear after taking antibiotics are caused by viruses-not the drug. For example, a child with mononucleosis who takes amoxicillin often gets a rash, but it’s not an allergy. This is why doctors need to consider timing, symptoms, and whether the patient had a recent infection before labeling it an allergy.
Should I carry an epinephrine auto-injector if I have a food allergy?
If you’ve had a severe reaction-like trouble breathing, swelling of the throat, or a drop in blood pressure-yes. Even if your last reaction was mild, future ones can be worse. Epinephrine is the only treatment that stops anaphylaxis. Don’t wait to use it. If you’re unsure, talk to an allergist about your risk.
Can I be allergic to both food and medication?
Yes. Having one type of allergy doesn’t protect you from another. Many people with food allergies also react to medications. The immune system can be sensitive in multiple ways. That’s why accurate diagnosis for each is critical-don’t assume one diagnosis explains all your symptoms.
What should I do if I think I had an allergic reaction?
Stop the substance immediately. If symptoms are severe-swelling, trouble breathing, dizziness-use epinephrine if you have it and call emergency services. Even if symptoms improve, go to the ER. Anaphylaxis can come back. Afterward, schedule an appointment with an allergist. Bring your symptom log and any medications you took. Don’t self-diagnose. Get it confirmed.

Comments
Joie Cregin January 18, 2026 AT 07:35
This post hit different. I used to think my rash after amoxicillin was an allergy until my allergist laughed and said it was probably mono. Turns out I can take penicillin just fine. So many people live with unnecessary fear because no one ever checked. Thanks for laying this out so clearly.
john Mccoskey January 18, 2026 AT 14:42
Let’s be real - the medical system is built on assumptions, not evidence. People get labeled allergic to penicillin based on a childhood rash from 1997 and then spend the rest of their lives on vancomycin because no one had the patience to test them. The cost isn’t just financial - it’s biological. Overuse of broad-spectrum antibiotics breeds superbugs. And yet, we still treat allergies like superstitions instead of diagnosable conditions. We need systemic change, not just individual awareness. The FDA’s new ImmunoCAP test is a start, but unless primary care providers are trained to refer, it’s just a shiny tool gathering dust in a lab somewhere.
brooke wright January 19, 2026 AT 03:28
I had a kid who broke out in hives after eating peanut butter and we panicked - turned out it was the palm oil in the cheap brand, not the peanuts. Now I log everything. Brand. Batch. Time. Even the weather. It’s weird but it works. Also, my sister thinks she’s allergic to ibuprofen because she gets headaches - nope, that’s just how her body reacts. Side effect ≠ allergy. So many people don’t get that.
Christina Bilotti January 19, 2026 AT 13:28
Of course you’re allergic to everything. Everyone is. It’s the new wellness trend. You can’t just have a stomachache anymore - now you have a ‘food sensitivity.’ You can’t take a pill without a rash and suddenly you’re ‘immune-compromised.’ People don’t want to accept that sometimes your body just reacts weirdly. It’s not an allergy, it’s bad luck. But hey, if labeling it as an allergy gets you a free epinephrine pen and a gluten-free cookie at Starbucks, who am I to judge?
Corey Chrisinger January 20, 2026 AT 09:52
It’s funny how we fear what we don’t understand. Allergies feel like a betrayal by your own body - like it’s turned against you. But what if it’s not betrayal? What if it’s just miscommunication? Your immune system isn’t evil - it’s confused. It sees a protein and thinks, ‘This looks like a parasite.’ So it screams. Loudly. And we call it an allergy. Maybe we need to stop treating our bodies like enemies and start listening to them like partners. Not every rash is a war. Sometimes it’s just a whisper.
Melodie Lesesne January 20, 2026 AT 17:44
I love how this breaks it down without jargon. My mom’s allergic to shellfish and I used to think it was just ‘being dramatic’ until I saw her go into anaphylaxis after a bite of shrimp. Now I carry two epinephrine pens in my bag. And I never assume a rash is ‘just a reaction.’ I ask: when? how? what else happened? It’s changed how I think about health.
Travis Craw January 21, 2026 AT 02:58
so i got a rash after amoxicillin when i was 12 and now im 34 and i still avoid all penicillins. but my doctor says maybe i should get tested. i dont know if i wanna risk it. what if i die? but what if i just wasted 20 years on worse antibiotics? idk. just wanted to say this post made me think.
Rob Deneke January 21, 2026 AT 06:48
Log everything. Even the little stuff. Brand. Time. What you ate before. Did you sleep? Were you stressed? Your body talks. You just gotta listen. And if you think you’re allergic to something get it checked. Don’t live in fear. Live with facts. Your life depends on it.
Bianca Leonhardt January 21, 2026 AT 22:04
Anyone who says they’re allergic to penicillin without testing is either lazy or lying. You think you’re being careful? You’re just making hospitals more expensive and yourself more vulnerable. Stop being a medical tourist and get tested. Your ignorance is costing lives.