When you're taking medication for osteoporosis, every minute matters. If you're also popping a magnesium supplement for muscle cramps, sleep, or just because you heard it’s good for you, you could be quietly sabotaging your treatment - and not even realize it.
Why Timing Between Magnesium and Osteoporosis Drugs Is Non-Negotiable
Bisphosphonates like Fosamax, Actonel, and Boniva are the most common pills prescribed for osteoporosis. They work by slowing down bone loss, helping your bones stay strong and less likely to break. But here’s the catch: these drugs are incredibly picky about what they’re mixed with in your stomach. Magnesium, whether it’s from a pill, antacid, or laxative, binds tightly to bisphosphonates. This isn’t just a minor inconvenience - it creates a chemical bond that turns the medication into an insoluble sludge your body can’t absorb. Studies show this can slash the effectiveness of your osteoporosis drug by up to 60%. That means six months of taking your pill faithfully could be completely wasted if you took your magnesium supplement just an hour before or after. The National Osteoporosis Foundation reports that over 10 million Americans have osteoporosis. For many, the goal is to avoid fractures - especially hip and spine fractures, which can be life-altering. If your medication isn’t working because of a timing mistake, you’re not just wasting money. You’re putting yourself at real risk.How Magnesium Kills Bisphosphonate Absorption
It’s not magic. It’s chemistry. Bisphosphonates have phosphonate groups - chemical structures that love to grab onto metal ions like magnesium (Mg²⁺). When magnesium enters your stomach at the same time as your osteoporosis pill, they latch on like two magnets. The resulting compound is too big and too heavy to pass through your intestinal wall into your bloodstream. This isn’t theoretical. The FDA’s own prescribing information for alendronate (Fosamax) cites clinical trials from Merck showing a 40-60% drop in absorption when magnesium is present. That’s not a small effect. That’s the difference between your drug working and not working at all. Even worse, you might not even know you’re taking magnesium. Antacids like Maalox or Milk of Magnesia? Those are loaded with magnesium. Laxatives? Often magnesium-based. Even some bottled waters, like San Pellegrino, contain noticeable amounts. If you’re taking any of these alongside your bisphosphonate, you’re risking treatment failure.The 2-Hour Rule - And Why It’s Not Just a Suggestion
The standard advice from every major medical group - the NIH, FDA, American Society for Bone and Mineral Research - is simple: wait at least two hours between taking your bisphosphonate and any magnesium product. But here’s the catch: the two hours aren’t just about the magnesium. Bisphosphonates themselves require strict rules. You have to take them first thing in the morning, on an empty stomach, with a full glass of water. Then you have to stay upright for at least 30 minutes. No coffee. No food. No other pills. So the full protocol looks like this:- First thing in the morning: Take your bisphosphonate with 8 oz of plain water.
- Wait 30 minutes before eating or drinking anything else.
- Wait another 90 minutes (so 2 full hours total) after taking the bisphosphonate.
- Then, and only then, take your magnesium supplement.
What About Natural Sources of Magnesium?
Some people ask: “What if I eat spinach, almonds, or black beans? Do I need to wait two hours after dinner too?” The short answer: no. The interaction only matters with supplemental magnesium - the kind you take in pill form, or in high-dose antacids and laxatives. Food-based magnesium is absorbed slowly and in much smaller amounts. It doesn’t create the same concentrated chemical environment that triggers the binding reaction. The American College of Rheumatology explicitly states that dietary magnesium doesn’t interfere with bisphosphonate absorption. So enjoy your kale salad and walnuts without worry. But if you’re taking a 400mg magnesium capsule at night? That’s the problem.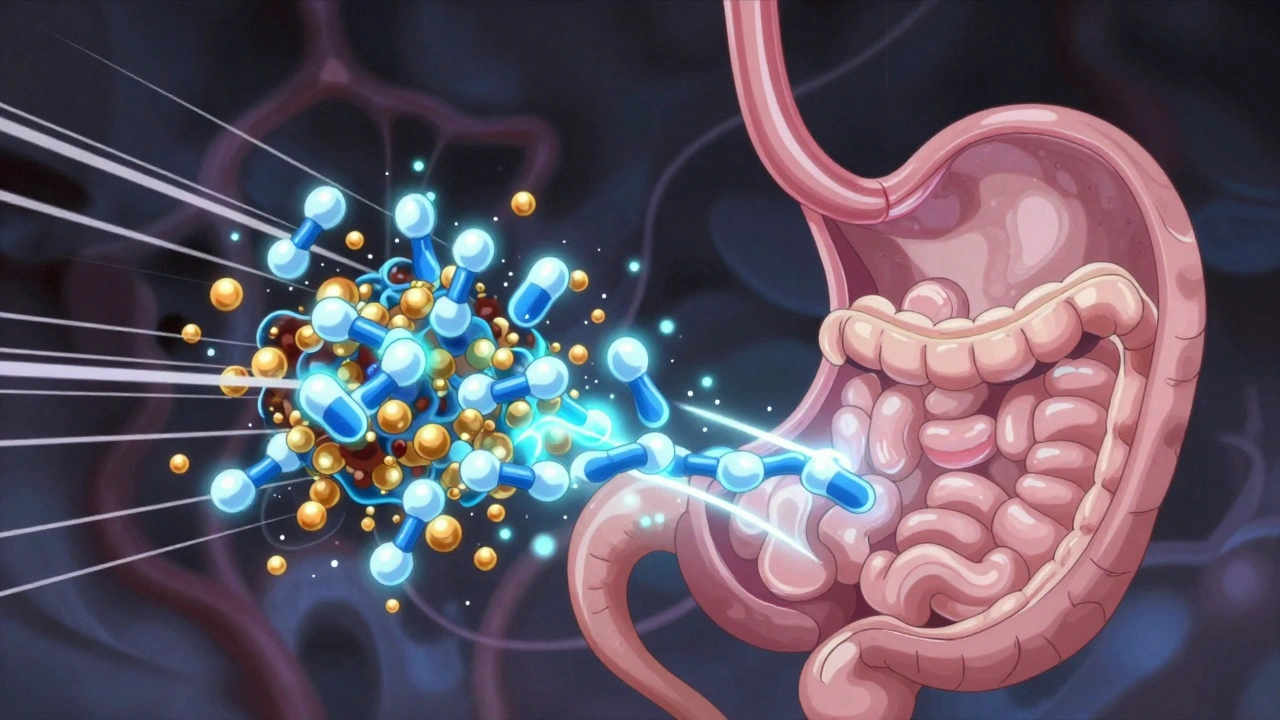
Real People, Real Mistakes
You’d think this would be common knowledge. But it’s not. A 2022 survey by the National Osteoporosis Foundation found that 37% of people taking both magnesium supplements and bisphosphonates didn’t know about the interaction. Over 20% admitted they took them together - sometimes within the same hour. One Reddit user, ‘BoneBuilder87’, shared that after taking Fosamax and magnesium for restless legs at the same time for six months, their bone density scan showed zero improvement. Another person on Drugs.com wrote that they didn’t realize Maalox counted as magnesium - until their doctor told them their bones were getting worse, not better. These aren’t rare stories. They’re common. And they’re preventable.How to Get It Right - Practical Tips
If you’re on bisphosphonates and take magnesium, here’s how to make sure you’re doing it right:- Use a pill organizer with four compartments. A standard AM/PM organizer won’t cut it. You need space to separate your morning bisphosphonate from your evening magnesium.
- Write it down. Keep a simple log: “7 AM: Fosamax. 9:30 AM: Breakfast. 10 PM: Magnesium.”
- Check every product. Look at the “Supplement Facts” label. If it says “magnesium” or “magnesium hydroxide,” “magnesium citrate,” or “magnesium oxide,” it counts.
- Ask your pharmacist. When you pick up your bisphosphonate, ask: “Does this interact with any magnesium products I take?”
- Use a timing wheel. Some pharmacies give out visual tools - a spinning dial that shows you the 2-hour window. One study found these boosted adherence by 67% compared to written instructions.
What About Other Osteoporosis Drugs?
Not all osteoporosis meds are affected. The timing rule only applies to oral bisphosphonates: alendronate, risedronate, ibandronate. If you’re on an intravenous drug like Reclast (zoledronic acid), you don’t need to worry. It goes straight into your vein - bypassing your stomach entirely. Same goes for denosumab (Prolia), which is a shot, not a pill. But if your doctor prescribed you a pill you take once a week or once a month? You’re on an oral bisphosphonate. The rule still applies.
The Bigger Picture: Why This Matters
This isn’t just about a pill. It’s about your long-term health. Osteoporosis fractures lead to chronic pain, loss of independence, and even higher risk of death - especially in older adults. Studies show patients who follow the 2-hour rule improve their bone density by 8.2% more over two years than those who don’t. That’s not a small difference. That’s the difference between walking without pain and needing a cane. Between living at home and moving to a care facility. The FDA calls this interaction a “preventable treatment failure mode” affecting nearly 1.8 million Americans every year. That’s not a number. That’s 1.8 million people who could have avoided fractures - if they’d just known to wait two hours.What’s Changing Soon
Good news: the system is catching up. By January 2025, all U.S. pharmacies will be required to use a standardized counseling script when dispensing bisphosphonates. Pharmacists will have to ask about magnesium - no exceptions. Newer bisphosphonate formulations are also in development. Merck’s ALN-103, currently in Phase 3 trials, is designed to be less affected by mineral interactions. Smart pill bottles with Bluetooth reminders - tested at Mayo Clinic - are already showing 92% adherence rates. But until those arrive, the rule stays the same: two hours apart.Final Checklist: Are You Doing It Right?
Before you go to bed tonight, ask yourself:- Did I take my bisphosphonate first thing in the morning - with water, on an empty stomach?
- Did I wait 30 minutes before eating or drinking anything else?
- Did I wait a full two hours before taking magnesium - even if it was just a sleep aid or antacid?
- Did I check the label of every supplement, OTC medicine, or bottled water I’ve taken today?
Can I take magnesium at night if I take my osteoporosis pill in the morning?
Yes - as long as you wait at least two full hours after taking your bisphosphonate. For example: take Fosamax at 7 AM with water, wait until 9 AM to eat, then take magnesium at 10 PM. The key is the two-hour gap after the bisphosphonate, not the time of day.
What if I forget and take them together by accident?
Don’t panic. One mistake won’t ruin your treatment. But don’t make it a habit. Skip your magnesium dose that day if you took your bisphosphonate too soon after. Resume the two-hour rule the next day. Consistency over time matters more than perfection.
Do all magnesium supplements have the same effect?
Yes. Whether it’s magnesium citrate, oxide, glycinate, or chloride - they all release magnesium ions in your stomach. That’s what binds to the bisphosphonate. The form doesn’t matter. The dose does. Even 100mg can interfere. Stick to the 2-hour rule regardless of the type.
Can I take calcium with my bisphosphonate?
No - calcium also interferes. Like magnesium, calcium binds to bisphosphonates and blocks absorption. Take calcium supplements at least two hours after your bisphosphonate, or better yet, get your calcium from food. Dairy, leafy greens, and fortified plant milks are safe.
Is it safe to take magnesium if I’m on Reclast or Prolia?
Yes. Reclast (zoledronic acid) is given by IV, and Prolia (denosumab) is a subcutaneous injection. Neither is absorbed through the gut, so magnesium supplements won’t affect them. You can take magnesium at any time - no timing rules needed.

Comments
Arjun Deva December 5, 2025 AT 20:05
So let me get this straight… the FDA, NIH, and every pharmacy in America are all in on this 2-hour lie? And you’re telling me I can’t take my magnesium with my Fosamax… but my neighbor’s cousin’s yoga teacher’s aunt swears she’s been taking them together for 12 years and her bones are “stronger than steel”? I mean… who’s really in control here? The doctors? Or Big Pharma’s secret magnesium suppression agenda??
Inna Borovik December 6, 2025 AT 18:13
Let’s be precise: the 60% absorption reduction is cited from Merck’s internal trials on alendronate - not a meta-analysis. And the FDA’s prescribing info? It’s a footnote. The real issue is that this interaction is clinically insignificant in low-dose magnesium (<100mg) and irrelevant if taken with food. The article conflates pharmacokinetics with fearmongering. Also - “bottled water contains noticeable amounts”? San Pellegrino has 58mg/L. You’d need to chug 7 liters to interfere. This is pseudoscience dressed as medical advice.
Jackie Petersen December 7, 2025 AT 08:23
AMERICA IS BEING GAMED. They want you to take expensive pills. They want you to wait two hours. They want you to buy fancy pill organizers. Meanwhile, in India, China, and Brazil - people just take their magnesium and their bones and live to 90. This whole thing is a capitalist scam to sell you more stuff. I took Fosamax and my magnesium gummies at the same time for 3 years - guess what? My hip didn’t break. My wallet did.
Annie Gardiner December 9, 2025 AT 03:37
Isn’t it funny how we’ve turned medicine into a ritual? You have to rise at dawn. Drink water. Stay upright. Wait two hours. Like you’re performing a sacred rite to the Bone Gods. But what if… what if your body just knows? What if the real problem isn’t magnesium… but our obsession with control? Maybe we don’t need to time everything. Maybe we just need to trust ourselves a little more.
Rashmi Gupta December 11, 2025 AT 01:38
I don’t trust any of this. The article says “studies show” - but doesn’t cite them. And who wrote this? A pharma rep? I take magnesium at night, Fosamax in the morning - no problem. My doctor never said anything. Why is this suddenly a crisis? I think they’re just trying to sell more supplements. I’m not changing my routine.
Max Manoles December 12, 2025 AT 20:47
Actually, the 2-hour rule is well-supported by pharmacokinetic studies. The gastric emptying time for oral bisphosphonates is ~30–60 minutes, but the drug remains bioavailable in the upper GI tract for up to 2 hours. Magnesium ions form insoluble complexes with phosphonates, reducing bioavailability by 40–60% - confirmed in randomized crossover trials. The advice isn’t arbitrary. It’s based on AUC and Cmax data. If you want to maximize efficacy, follow the protocol. Your bones will thank you.
Katie O'Connell December 13, 2025 AT 15:32
It is, regrettably, both lamentable and unsurprising that such a nuanced pharmacological interaction has been reduced to a viral Reddit post replete with bullet points and emotive exhortations. The article, while superficially informative, lacks critical engagement with the primary literature, fails to contextualize the clinical significance of the interaction, and indulges in alarmist rhetoric that undermines the very authority it purports to uphold. One would hope for peer-reviewed rigor, not bullet-pointed panic.
Kumar Shubhranshu December 15, 2025 AT 14:36
I took Fosamax and magnesium together for 4 years. My BMD went up 5%. My doctor said I'm fine. You're overcomplicating this.
Mayur Panchamia December 16, 2025 AT 07:04
YOU THINK YOU’RE SMART? YOU THINK YOU KNOW BETTER THAN THE FDA? YOU THINK YOUR “I’VE BEEN DOING IT WRONG FOR YEARS AND I’M FINE” STORY MEANS SOMETHING? YOU’RE A WALKING OSTEOPOROSIS TIKTOK VIDEO! I’M TAKING MY MAGNESIUM AT 10 PM - TWO HOURS AFTER MY 7 AM FOSAMAX - AND I’M PROUD OF IT! DON’T BE A SHEEP! FOLLOW THE RULES OR BREAK YOUR HIPS! AMERICA NEEDS DISCIPLINE - NOT “TRUST YOUR BODY” CULTURE!