When you're on Medicaid, getting your prescriptions shouldn't be a maze. But if you've ever been told your medication isn't covered, had to try two other drugs first, or waited weeks for approval, you know it can feel like one. The truth is, Medicaid does cover prescription drugs - but not all drugs, and not always the way you expect. In 2026, coverage depends heavily on where you live, what drug you need, and whether it’s on your state’s preferred list.
Medicaid Covers Prescriptions - But Only If They’re on the List
Every state runs its own Medicaid program, but they all follow the same basic rule: prescription drugs are covered, but not everything. States create a Preferred Drug List (PDL), also called a formulary, that says exactly which medications they’ll pay for without extra steps. Think of it like a menu - you can order anything on it, but if you want something off-menu, you need permission.
By 2025, every state and D.C. covered outpatient prescriptions for nearly all Medicaid enrollees. That’s about 85 million people. But what’s covered? It’s not random. Generic drugs are almost always included. Brand-name drugs? Maybe. New, expensive specialty drugs? Only if they meet strict criteria.
For example, in North Carolina, drugs like Vasotec, Trulance, and Uceris were removed from the formulary in 2025 because they no longer offered enough rebate savings. Meanwhile, Epidiolex® - a drug for severe epilepsy - was moved from "preferred" to "non-preferred," meaning patients now need prior authorization just to get it.
How Tiers Work: Generics First, Then Brands
Most state formularies use a tier system. It’s simple:
- Tier 1: Generic drugs. Lowest cost to you - often $0 to $5 per prescription.
- Tier 2: Brand-name drugs. Higher copay - usually $10 to $40.
- Tier 3: Specialty drugs. These are high-cost medications for conditions like cancer, MS, or rheumatoid arthritis. Copays can hit $100 or more.
Here’s the catch: even if a brand-name drug is on the list, you might still have to try the generic first. This is called "step therapy" or "trial and failure." In 38 states, you must fail two preferred drugs before they’ll cover the third - even if your doctor says the first two didn’t work or caused side effects.
Take SSRIs for depression. In North Carolina, you might need to try two different generics before they approve Wellbutrin XL. If your doctor says you tried them both and they made you feel worse? You still need paperwork. That paperwork - a prior authorization - can take 7 to 14 days to get approved. And if it’s denied? You appeal. Of the appeals with full medical notes, 78% get overturned.
Prior Authorization: The Hidden Hurdle
Prior authorization isn’t just a form. It’s a barrier. It requires your doctor to submit clinical notes, lab results, or proof that cheaper options failed. Some states require it for everything. Others only for high-cost or high-risk drugs.
For example, North Carolina requires prior authorization for premixed insulin in Type 1 Diabetes patients - but only if it’s not the first time they’re prescribed it. And once approved, that authorization lasts up to three years. That’s good news if you’re stable. But if your condition changes? You’re back to square one.
According to the Medicare Rights Center’s 2024 survey, 63% of Medicaid beneficiaries experienced delays because of prior authorization. Average wait time? Over a week. For someone with chronic pain or diabetes, that delay can mean hospital visits, worse symptoms, or even emergency care.
What’s Not Covered - And Why
Not every drug is eligible. Some are excluded outright:
- Drugs that don’t offer enough rebate to the state
- Drugs with no generic equivalent and extremely high list prices
- Over-the-counter medications (unless prescribed for a specific condition)
- Drugs used for cosmetic reasons (like hair growth treatments)
- Drugs not approved by the FDA
States remove drugs from their lists all the time - usually because the manufacturer stopped offering a rebate. In 2025, North Carolina removed 12 drugs from its formulary because they no longer met the state’s rebate threshold. That’s not a mistake. It’s policy.
There’s also the Federal Upper Limit (FUL). This rule caps how much Medicaid will pay for generic drugs. It’s calculated at 250% of the average manufacturer price minus 17.1%. If a generic drug costs more than that cap, Medicaid won’t cover it - even if it’s the only option. That’s why some patients get switched to a different generic, even if it’s not their usual brand.
Extra Help: A Lifeline for Low-Income Beneficiaries
If you’re on Medicaid, you might qualify for "Extra Help" - a federal program that cuts your Medicare Part D drug costs even further. It’s automatic if you get full Medicaid coverage, SSI, or state help with Medicare premiums.
Here’s what Extra Help does in 2026:
- $0 monthly premium
- $0 deductible
- Max $4.90 copay for generics
- Max $12.15 for brand-name drugs
- Once you hit $2,000 in total drug costs, you pay $0 for the rest of the year
That’s huge. The Medicare Rights Center found that 89% of people with Extra Help were satisfied with their drug costs - compared to just 42% without it. But here’s the problem: about 1.2 million people who qualify don’t even know they’re eligible. If you’re on Medicaid, check if you’re getting Extra Help. You might not even realize you’re already enrolled.
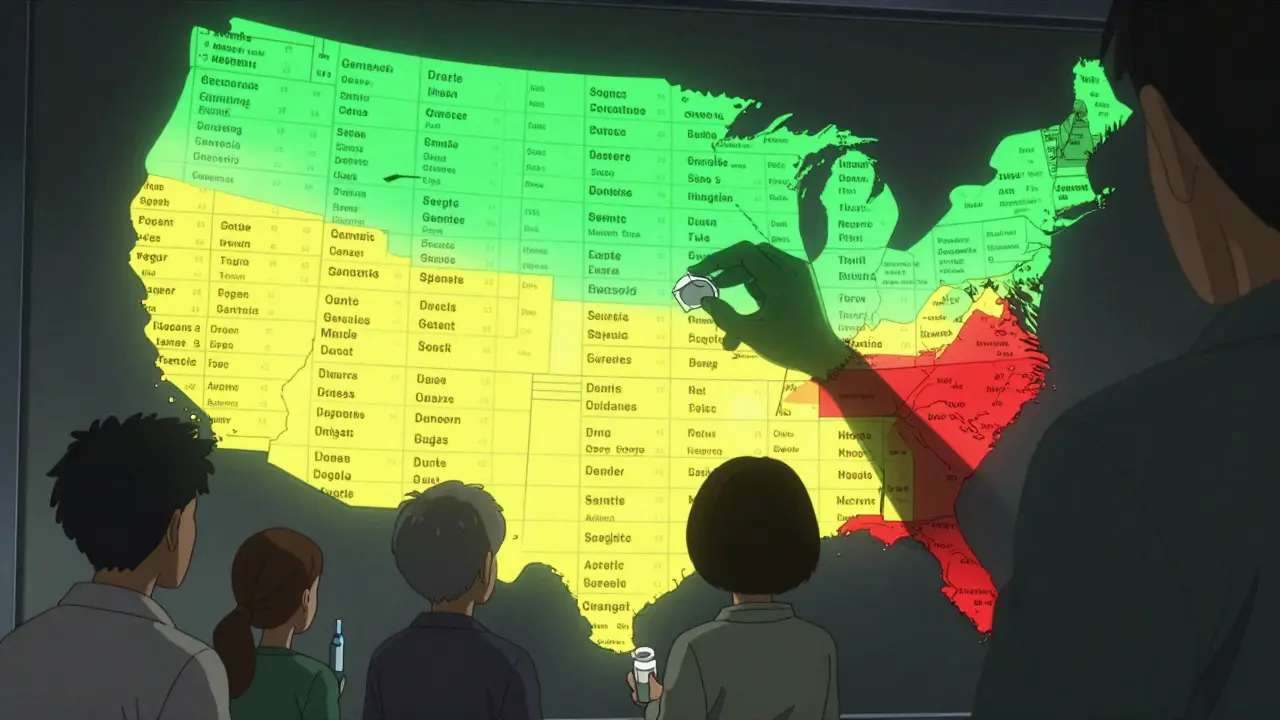
State-by-State Differences Matter
North Carolina requires two-step failure before covering non-preferred drugs. Florida has a separate quick-reference guide for physician-administered drugs. Some states allow exceptions for pregnancy, mental health, or rare diseases. Others don’t.
There are 50 different formularies. That means your drug might be covered in Georgia but not in Alabama. A drug your doctor prescribes in Texas might be blocked in Ohio. That’s why you can’t rely on national websites alone. You need to check your state’s official Medicaid website - or call your state’s SHIP (State Health Insurance Assistance Program) office.
Pharmacy benefit managers (PBMs) like CVS Caremark, Express Scripts, and OptumRx run these formularies for states. But they don’t make the rules - states do. So if you’re denied coverage, the answer isn’t "call the pharmacy." It’s "call your state Medicaid office." They’re the ones who decide what stays on the list.
What You Can Do
Here’s how to navigate this system without getting stuck:
- Know your formulary. Go to your state’s Medicaid website. Search for "Preferred Drug List" or "Formulary." Download it. Look up your medication.
- Ask about tier and step therapy. If your drug is on Tier 2 or 3, ask if you need to try others first. If yes, ask what the alternatives are.
- Get your doctor involved. If you’re denied, ask your doctor to write a letter of medical necessity. Include why previous drugs failed. Attach lab results or side effect logs.
- Use in-network pharmacies. Out-of-network pharmacies won’t process your claim. Mail-order services often have lower copays for maintenance meds.
- Check for Extra Help. Even if you’re on Medicaid, you might not know you’re enrolled. Call 1-800-MEDICARE or visit Medicare.gov.
And remember: rules change. Formularies get updated in July, October, and sometimes mid-year. What was covered last month might not be covered next month. Stay alert. Bookmark your state’s Medicaid pharmacy page. Sign up for email alerts if they have them.
Costs Are Rising - But So Are Protections
Medicaid spends $64.3 billion a year on prescriptions. Specialty drugs - like gene therapies that cost over $2 million per dose - are driving that growth. In 2026, CMS is rolling out new rules to prevent states from blocking access to medically necessary drugs. That’s a win.
Also, starting in 2025, Medicaid and Extra Help beneficiaries can change their drug plan once a month instead of waiting for the annual enrollment period. That’s huge. If your drug gets dropped, you can switch faster.
But the system is still fragile. A single drug removal can leave a patient without treatment. A slow prior auth process can lead to a hospital stay. The goal is to save money - but not at the cost of health.
If you’re struggling to get your meds, you’re not alone. And you’re not powerless. Know your rights. Use your doctor. Ask for help. And don’t give up on the appeal.
Does Medicaid cover all prescription drugs?
No. Medicaid covers most prescription drugs, but each state has its own formulary - a list of approved medications. Some drugs are excluded because they don’t offer enough rebate savings, aren’t FDA-approved, or are considered non-essential (like cosmetic treatments). Even if a drug is FDA-approved, it may not be on your state’s list.
Why do I have to try other drugs before getting mine?
This is called "step therapy" or "trial and failure." States use it to control costs. They require you to try cheaper, preferred drugs first - usually two - before covering a more expensive one. Exceptions exist for certain conditions (like pregnancy or rare diseases), but you’ll need documentation from your doctor to qualify.
What if my drug gets removed from the formulary?
If your drug is removed, you may still get it through prior authorization if you can prove medical necessity. Some states allow temporary coverage while you switch to an alternative. You can also appeal the decision - especially if your doctor provides clinical evidence. Check your state’s Medicaid website for appeal procedures.
Can I use any pharmacy with Medicaid?
No. You must use pharmacies in your state’s Medicaid network. Out-of-network pharmacies won’t be able to process your claim. Many states encourage or require mail-order pharmacies for maintenance medications (like blood pressure or diabetes drugs) because they offer lower copays and better savings.
Do I qualify for Extra Help if I’m on Medicaid?
Yes - if you have full Medicaid coverage, receive SSI payments, or get help paying your Medicare Part B premium, you automatically qualify for Extra Help. This program lowers your drug costs to $0 premiums, $0 deductibles, and maximum $4.90 copays for generics. About 1.2 million eligible people don’t realize they qualify. Check your status at Medicare.gov or call 1-800-MEDICARE.
How often do Medicaid formularies change?
Formularies are updated at least twice a year - often in July and October - but states can make changes mid-year if drug rebates change or new drugs are approved. North Carolina, for example, made three updates in 2025. Always check your state’s Medicaid website for the latest version. Don’t assume last year’s list still applies.
What’s the difference between Medicaid and Medicare Part D drug coverage?
Medicaid is state-run and covers low-income individuals of all ages. It has no annual cap on drug costs and often includes Extra Help automatically. Medicare Part D is federal, run by private insurers, and designed for seniors and disabled people. It has a $2,000 out-of-pocket cap (in 2026), but costs can still be high without Extra Help. If you’re dual-eligible (Medicaid + Medicare), Medicaid usually pays for drugs not covered by Part D.

Comments
Mike Hammer February 15, 2026 AT 11:28
I got my insulin denied last month because it wasn't on the list. Took three weeks and three letters from my doctor just to get it back. Meanwhile, my blood sugar went haywire. This system is broken. Not even a joke.
Daniel Dover February 17, 2026 AT 05:42
This is exactly why I moved back to the UK. At least here, if a doctor says you need it, you get it.
Virginia Kimball February 17, 2026 AT 11:38
I used to think Medicaid was a safety net until I spent 47 days fighting for my antidepressant. Now I call it a labyrinth with a side of bureaucracy. My therapist said I needed Wellbutrin. They made me try three generics first. Two gave me panic attacks. The third made me feel like a zombie. Still had to appeal. 78% get approved? That’s cold comfort when you’re stuck in the middle of it.
Michael Page February 19, 2026 AT 11:25
The real issue isn't the formulary. It's the assumption that cost containment equates to rational care. We've turned pharmacology into a spreadsheet. A human life is not a line item. The FDA approves drugs based on efficacy and safety. Medicaid denies them based on rebate percentages. That's not policy. That's moral bankruptcy dressed up as fiscal responsibility.
Betty Kirby February 21, 2026 AT 08:57
People act like this is some new horror show. Newsflash: it's been like this for a decade. You think your doctor has your back? They're just as trapped. They have to fill out forms that make IRS paperwork look like a haiku. And don't get me started on PBMs. They're the middlemen who profit from the chaos. You're not fighting the state. You're fighting a corporate shell game.
Josiah Demara February 23, 2026 AT 06:39
You people are pathetic. If you can't afford your meds, don't take them. Or better yet, don't get sick. Medicaid isn't a buffet. You don't get to pick the expensive entree just because your doctor has a favorite brand. I've seen people on SSI with 17 prescriptions. That's not healthcare. That's addiction to the system. Stop whining and take a generic. Your body didn't evolve for brand names.
Charlotte Dacre February 23, 2026 AT 10:41
So let me get this straight. You need a prescription for insulin, but the state says no unless you've first tried three cheaper versions that literally don't work for you? And this is considered "smart cost control"? I'd like to see someone explain this to a diabetic child. Or better yet, explain it to their parent who's working two jobs and still can't afford the copay. Oh wait-you can't. Because you're too busy counting rebates.
Esha Pathak February 23, 2026 AT 16:33
In India, we don’t have Medicaid. We have hope. And sometimes, just hope. My cousin’s daughter has epilepsy. She gets Epidiolex. We pay out of pocket. $12,000 a month. We sell jewelry. We borrow from cousins. We cry. We pray. We don’t have formularies. We have love. And desperation. I wish you all had that. At least then you’d know what real sacrifice looks like.
Chiruvella Pardha Krishna February 24, 2026 AT 03:36
The tragedy is not that drugs are excluded. The tragedy is that we have accepted this as normal. We have normalized bureaucratic cruelty. We have convinced ourselves that a $4.90 copay is a victory when the system that enabled it demanded a person suffer before being granted relief. This is not healthcare. This is performance art. And we are all complicit in the script.
Joe Grushkin February 25, 2026 AT 23:01
Medicaid is a program. Not a right. If you want guaranteed access to every drug your doctor prescribes, go make more money. Or move to Canada. Or Switzerland. Or Mars. This isn't a failure of policy. It's a failure of ambition. Stop expecting the government to fund your personal pharmaceutical wishlist.
Mandeep Singh February 26, 2026 AT 18:35
I've worked in pharmacy for 18 years. I've seen people cry because they couldn't get their blood pressure med. I've seen elderly women skip doses so their grandkids could eat. I've seen doctors write appeals so detailed they looked like dissertations. And I've seen 9 out of 10 get denied. This isn't about savings. It's about control. The state doesn't care if you die. They care if the rebate drops below 18%. That's the metric. Not your life. Not your pain. Not your sleepless nights. Just the number. And they'll move heaven and earth to keep it.
Kaye Alcaraz February 27, 2026 AT 10:16
To all who are struggling: please reach out to your State Health Insurance Assistance Program. You are not alone. Many of you are already eligible for Extra Help and do not know it. Your state's SHIP office provides free, confidential counseling. They can help you appeal denials, understand your formulary, and connect you with patient assistance programs. You have rights. Use them. You deserve care.
Sarah Barrett February 27, 2026 AT 10:48
I appreciate the thorough breakdown. The tier system and prior authorization details are particularly useful. It's clear that state-level variation creates significant disparities. I'd add that patients should also request a copy of their formulary in writing-some states only post PDFs that change without notice. Keeping a printed version helps when disputing denials.
Erica Banatao Darilag February 27, 2026 AT 14:56
i got my meds denied last week and i didnt even know why. i called the number on the back of my card and they put me on hold for 45 min. then they said "we cant help you with that". i think i might have a typo in my name. or maybe my insurance just gave up. either way i feel like a ghost.
Kapil Verma March 1, 2026 AT 12:48
This is why America is falling apart. You people cry about a $10 copay while India and China build empires. We spend billions on drugs that don't even work. Why not just give people aspirin and tell them to pray? At least that doesn't cost the government a dime. You want help? Stop being weak. Get a job. Move to a state that actually works. This is why we lost to China.