When your child comes home from swim class with a few tiny, pearly bumps on their arm, it’s natural to panic. Are these warts? Are they contagious? Will they scar? The truth is, those little bumps are likely molluscum contagiosum - a common, harmless viral skin infection that affects millions of kids every year. Despite how alarming they look, most cases clear up on their own without treatment. But knowing what to do - and what not to do - makes all the difference.
What Exactly Is Molluscum Contagiosum?
Molluscum contagiosum is caused by a virus called MCV, part of the poxvirus family. It’s not dangerous, not cancerous, and doesn’t lead to long-term health problems in healthy people. The virus creates small, round bumps on the skin - usually 2 to 6 millimeters across - with a dimple or dot in the center. They can be white, pink, or skin-colored, and often look like little pearls. These bumps aren’t painful, but they can itch, especially if the person has eczema. The virus spreads easily through direct skin contact. Think sharing towels, hugging, playing sports, or even swimming in a pool. Kids get it from other kids at school or daycare. Adults usually catch it through sexual contact. If someone has eczema, they’re 30% more likely to get molluscum because their skin barrier is already compromised. The incubation period is 2 to 6 weeks, so you won’t see bumps right after exposure.How Is It Different From Other Skin Issues?
Many people mistake molluscum for warts, herpes, or chickenpox. But here’s how to tell them apart:- Warts (HPV) are rough, raised, and lack the central dimple. They’re firmer and often appear on fingers or feet.
- Herpes causes painful blisters that break open and crust. Molluscum bumps are firm and don’t hurt.
- Chickenpox spreads all over the body and includes fluid-filled blisters that turn into scabs. Molluscum stays localized and doesn’t change shape quickly.
- Impetigo is bacterial, oozes, and forms honey-colored crusts. Molluscum stays dry and intact.
Why Most Cases Don’t Need Treatment
The American Academy of Dermatology says the best treatment for healthy children is no treatment at all. Why? Because molluscum usually goes away on its own in 6 to 24 months. Studies show 92% of cases clear up within 18 months without leaving scars. Aggressive treatments like freezing, scraping, or burning can cause pain, redness, and even scarring - especially on the face. Dr. Adam Friedman, a leading dermatologist, says: “The bumps are more of a nuisance than a threat. Treating them aggressively often does more harm than good.” Parents often feel pressured to “do something.” But watching and waiting is not neglect - it’s evidence-based care. The CDC updated its guidelines in 2023 to say: “No child should be kept out of school or swimming because of molluscum.”When Treatment Might Make Sense
There are times when treatment is worth considering:- Lesions on the face or genitals that cause emotional distress or bullying
- Large clusters that keep spreading despite hygiene measures
- Children with weakened immune systems (like those with eczema or HIV)
- Teenagers or adults with genital bumps who want to avoid spreading it to partners
- Cantharidin - a blistering agent applied by a doctor. It causes a small blister to form, lifting the bump off. Studies show 73% clearance after 12 weeks.
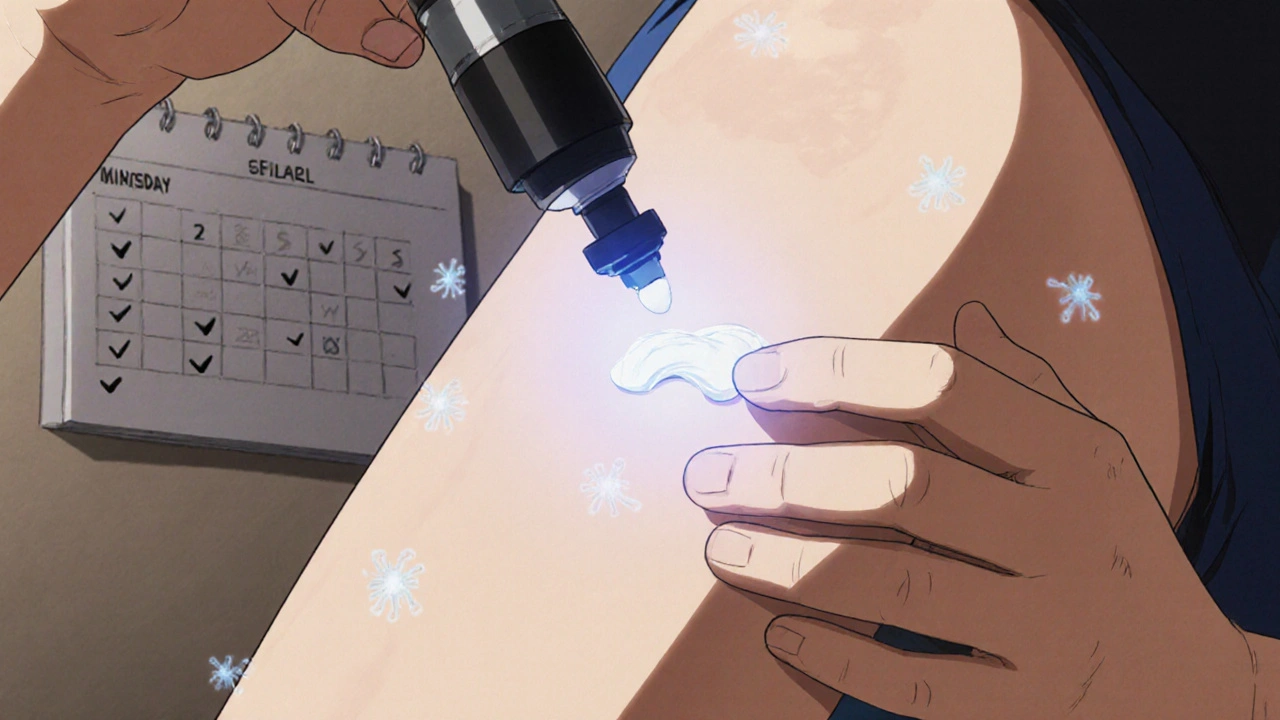
- Topical potassium hydroxide - available in over-the-counter creams like MolluDab. Used daily, it clears lesions in about 8 weeks for 63% of users.
- Cryotherapy - freezing with liquid nitrogen. Effective but can be painful and risky on delicate skin. Many parents regret this choice for facial bumps.
- Immunomodulators - new topical drugs in clinical trials (like those tested in NCT05217892) are showing 82% clearance, but aren’t widely available yet.
How to Stop It From Spreading
Prevention is easier than treatment. Here’s what actually works:- Don’t share towels, clothing, or toys. One CDC study showed this cuts household spread by 57%.
- Cover bumps during swimming. While the virus can survive in water, most pools are chlorinated enough to kill it. Still, many swim programs require coverage to avoid complaints from other parents.
- Keep nails short and discourage scratching. Scratching spreads the virus to other parts of the body. Mayo Clinic data shows scratching can triple the number of bumps.
- Wash hands often. Simple, but effective. Especially after touching bumps or applying cream.
- Use separate bath time. If you have multiple kids, bathe the infected child last and clean the tub afterward.
What Parents Are Really Doing
Real-world behavior tells a different story than medical guidelines. A BabyCenter survey of 452 parents found 78% chose no treatment. They watched, waited, and focused on hygiene. Only 12% used over-the-counter creams. Just 10% went for doctor procedures. But on Reddit and parenting forums, the emotional toll shows up. One user, “MolluscumSurvivor69,” shared how genital bumps caused 14 months of anxiety before they cleared. Another parent wrote: “I felt judged at the playground. No one said anything, but I could feel it.” That’s why some doctors now recommend early treatment for visible facial bumps - not for medical reasons, but for mental health. A 2021 study found 45% of school-aged kids with facial molluscum experienced teasing or social withdrawal.What Doesn’t Work (And Can Hurt)
There are tons of “miracle cures” online: tea tree oil, apple cider vinegar, duct tape, iodine. None of these are proven to work. Worse, some cause chemical burns or allergic reactions. The FDA issued a warning in 2022 to three companies selling unregulated molluscum creams with no dosage instructions. One product had potassium hydroxide at 20% - far above the safe 5-10% range. That’s dangerous for kids. Also avoid aggressive procedures like laser removal or curettage (scraping) for young children. The pain, trauma, and risk of scarring outweigh the benefits.
What’s New in 2025?
The field is slowly changing. A new topical immunomodulator showed 82% clearance in a 2023 clinical trial. It’s not on the market yet, but it’s the most promising development in years. The CDC’s 2023 update was a big win: schools and pools can’t exclude kids with molluscum anymore. That’s helping reduce stigma. Global trends suggest cases may rise 22% over the next decade due to warmer, more humid climates - especially in tropical regions where prevalence already hits 18% in kids.When to See a Doctor
You don’t need to rush to the dermatologist for every bump. But call if:- The bumps are growing rapidly or spreading beyond a few areas
- They become red, swollen, or ooze pus (sign of bacterial infection)
- Your child has eczema, HIV, or another immune condition
- Bumps appear on the eyelids or genitals and cause discomfort
- You’re unsure if it’s molluscum or something else
Final Thoughts: Patience Is the Best Medicine
Molluscum contagiosum is not a crisis. It’s a temporary skin glitch. It doesn’t mean your child is dirty. It doesn’t mean you failed as a parent. It’s just a virus - one that millions of kids get every year and outgrow without a trace. Focus on keeping the skin clean, avoiding scratching, and not sharing personal items. Give it time. Most bumps will vanish without a scar, without a procedure, and without drama. If you’re stressed, use the American Academy of Dermatology’s free “Molluscum Manager” app. It tracks bumps, sends reminders for hygiene, and gives you science-backed answers - not fear.Are molluscum bumps contagious?
Yes. Molluscum contagiosum spreads through direct skin contact or touching contaminated items like towels, toys, or pool equipment. It’s especially easy to spread among children in close settings like daycare or sports teams. The virus can survive on surfaces for hours, so hygiene is key to stopping transmission.
Will molluscum leave scars?
Usually not. In healthy children, the bumps resolve on their own without scarring. But aggressive treatments like freezing, scraping, or using strong chemicals can cause permanent marks. Scratching the bumps also increases the risk of scarring and secondary infection.
How long does molluscum last?
Most cases clear up in 6 to 24 months. About 92% resolve within 18 months without treatment. In rare cases, especially in people with weakened immune systems, bumps can last up to 4 years. The virus doesn’t become resistant - it just takes time for the body to fight it off.
Can adults get molluscum contagiosum?
Yes. Adults usually get it through sexual contact, especially if they have multiple partners. Bumps often appear on the genitals, inner thighs, or lower abdomen. In adults, the infection can be more persistent and may require treatment to prevent spreading to partners. Immunocompromised adults (like those with HIV) can develop widespread, large lesions that need medical attention.
Should my child stay home from school or swimming?
No. According to the CDC’s 2023 guidelines, children with molluscum should not be excluded from school, daycare, or swimming pools. The virus spreads slowly, and keeping kids home doesn’t stop outbreaks - it just causes unnecessary stress. Covering bumps with waterproof bandages during swimming is recommended, but isolation is not.
Is there a vaccine for molluscum contagiosum?
No, there is currently no vaccine available. Prevention relies on good hygiene, avoiding skin-to-skin contact with infected areas, and not sharing personal items. Research is ongoing, especially for immunocompromised populations, but no vaccine is in late-stage trials as of 2025.
Can molluscum come back after it clears?
Yes, but it’s uncommon. Once the body clears the virus, most people develop immunity and won’t get it again. However, since there are different strains of the molluscum virus, it’s possible - though rare - to get infected with a different strain later. This is more likely in people with weakened immune systems.
What’s the best over-the-counter treatment?
The most effective OTC option is a topical cream with 5-10% potassium hydroxide, like MolluDab. Used daily, it clears lesions in about 8 weeks for 63% of users. Avoid unregulated products with unknown ingredients. Tea tree oil, vinegar, and duct tape are not proven and can irritate skin. Always check with a doctor before using any topical treatment on a child.


Comments
Koltin Hammer November 17, 2025 AT 05:06
So many parents panic like their kid just got diagnosed with a terminal illness. Molluscum? It’s a viral pimple party. The body’s got this. I’ve seen kids with 50 bumps by June and zero by December. No treatment, no drama. Just let nature do its thing. The real tragedy? Parents burning their kid’s skin with cantharidin because they can’t handle the look of it. 🤷♂️
kanishetti anusha November 18, 2025 AT 14:54
I’m from India, and here we just use neem paste. Not scientific, but gentle. My nephew had it for 10 months-no treatment, just coconut oil and patience. No scars. No tears. Just a quiet victory.
Patrick Merk November 18, 2025 AT 20:57
My daughter got this after swim camp. We covered the bumps with waterproof bandages, kept her in the pool, and ignored the side-eye from other moms. One day, poof-gone. No doctor, no cream, no trauma. The real enemy isn’t the virus-it’s the guilt we project onto ourselves as parents. We’ve been sold fear as a product. Time to unbuy it.
Eric Gregorich November 19, 2025 AT 12:34
Let me tell you something about modern parenting: we’ve turned every minor skin glitch into a cosmic test of our worth. Molluscum isn’t a crisis-it’s a rite of passage. Like learning to tie shoes or surviving a sibling’s birthday party. We’re so obsessed with control that we’ve forgotten how to trust biology. The body isn’t broken. It’s learning. And if you’re treating it like a crime scene with cryotherapy and potassium hydroxide, you’re not protecting your child-you’re performing trauma on a tiny human who just wants to play tag. The CDC says they can swim. The dermatologists say leave it alone. But the internet? The internet sells you a $47 ‘molluscum destroyer’ cream with 17 ingredients you can’t pronounce. And you buy it. Because you’re scared. And fear sells. Always has. Always will.
Connor Moizer November 19, 2025 AT 16:03
Stop letting the internet make you paranoid. If your kid has a few bumps, cover them, wash hands, and move on. No need to turn this into a medical thriller. I’ve seen moms cry over this. Really. CRY. Like their kid has leprosy. It’s a virus. It’s not HIV. It’s not cancer. It’s just… skin. Chill the f*** out. Your kid’s gonna be fine.
roy bradfield November 20, 2025 AT 05:54
They’re lying to you. The CDC? The AAP? All part of the pharmaceutical-industrial complex. Why? Because if you don’t treat molluscum, you don’t need expensive creams, doctor visits, or laser treatments. The real agenda? Keep parents hooked on fear and overpriced ‘solutions.’ I’ve tracked this for years. There’s a hidden patent on a ‘natural’ cure that was buried in 2021. Tea tree oil? They say it doesn’t work. But it’s been used in Ayurveda for 5,000 years. Coincidence? I think not. They don’t want you to know that simple hygiene and time are the only real cures. Because that’s not profitable.
Liam Dunne November 21, 2025 AT 23:34
My niece had molluscum for 14 months. We did nothing. Just kept her nails trimmed and avoided sharing towels. One day, they just… disappeared. No scarring. No drama. The only thing that changed? My anxiety. The virus didn’t need fixing. I did.
Phil Best November 22, 2025 AT 10:26
Let me get this straight: we’re okay with kids getting chickenpox, measles, even hand-foot-and-mouth-but the second they get a few harmless little bumps, we’re scheduling cryotherapy appointments like it’s a Black Friday sale? What happened to us? We used to let kids be kids. Now we treat every pimple like a national emergency. I’m not saying don’t care. I’m saying stop turning parenting into a horror movie.
Vera Wayne November 24, 2025 AT 05:25
I just want to say-thank you-for writing this with such clarity. So many parents are drowning in misinformation. You didn’t just explain the science-you gave us permission to breathe. I’m printing this out and taping it to my fridge.
Rodney Keats November 25, 2025 AT 00:22
Oh, so now we’re supposed to just ‘wait’ while our kid’s covered in little pearl-looking tumors? And you call that ‘evidence-based’? Please. My neighbor’s kid got laser treatment and now has a scar the size of a dime. You think that’s better than 18 months of ‘patience’? You’re not protecting them-you’re gambling with their skin.
Koltin Hammer November 25, 2025 AT 17:07
And yet, 92% of kids clear it without scars. The ones with scars? Usually from parents panicking and trying to ‘fix’ it with something aggressive. The virus doesn’t care about your timeline. Your kid’s body does. Trust it.
Laura-Jade Vaughan November 26, 2025 AT 18:25
OMG I’m so glad someone finally said this!! 🙌 I’ve been so stressed about my daughter’s bumps, but this post made me cry-happy tears!! I’m gonna stop googling and just let it be 💖✨ #MolluscumIsNotAFailure
Willie Randle November 28, 2025 AT 08:48
Grammatically, the post is flawless. Structurally, it’s a model of clarity. But emotionally, it’s a lifeline. For every parent who’s been made to feel like a bad caregiver because their child has a few harmless bumps-this is your validation. You didn’t fail. The virus did. And it’s losing.