When your nails start looking weird-yellow, thick, crumbly, or lifting off the nail bed-it’s easy to assume it’s just a fungal infection. But what if it’s not? What if it’s something deeper, something tied to your immune system? Nail disorders like fungal infections and psoriatic changes look similar, but they’re completely different conditions. And mixing them up can cost you time, money, and even worse, make your nails worse.
What You’re Actually Seeing
Fungal nail infections, called onychomycosis, are caused by tiny organisms like Trichophyton rubrum. These fungi love warm, damp places. They start as a small white or yellow spot under the tip of your nail and creep slowly toward the cuticle over months. The nail gets thick, brittle, and often turns brown or black. About 90% of cases show darkening, and 40% give off a foul smell-something psoriasis never does. Nail psoriasis, on the other hand, isn’t an infection. It’s an autoimmune condition. Your body attacks its own skin cells, making them grow too fast-every 3 to 4 days instead of every 28 to 30. This messes up your nail matrix, the area under your cuticle where nails are made. You might notice tiny pits, like pinpricks, on your nail surface. That’s the most telling sign: 70% of people with nail psoriasis have them. You might also see salmon-colored patches under the nail, or a chalky buildup underneath. The nail can separate from the bed, but it doesn’t usually smell bad.The Big Differences You Can Spot
Here’s how to tell them apart without a lab test:- Nail pitting: Found in 78% of psoriasis cases, but only 2% of fungal infections. If you see little dents on your nail surface, it’s likely psoriasis.
- Foul odor: Present in 40% of fungal cases, zero in psoriasis. If your nail smells like old cheese, it’s probably fungal.
- Where it starts: Fungal infections begin at the tip or sides. Psoriasis often hits multiple nails at once, especially fingernails (75% of cases).
- Thickening: Fungal nails get thick-3 to 5 millimeters. Psoriatic nails thicken too, but usually only 2 to 3 millimeters.
- History: If you’ve had psoriasis on your skin or scalp for years, and now your nails are changing, it’s almost certainly psoriatic. Over 95% of nail psoriasis cases happen in people who already have skin psoriasis.
But here’s the catch: 68% of nail psoriasis cases look yellow, just like fungal infections. That’s why so many people get it wrong.
Why Misdiagnosis Is So Common-and Costly
Most people go to their doctor with a weird nail and say, “I think I have fungus.” Doctors, especially general practitioners, aren’t trained to spot the subtle signs. A 2023 JAMA Dermatology study found primary care doctors correctly diagnose these conditions only 52% of the time. Dermatologists? 85%. That gap means thousands of people are treated for the wrong thing. On Reddit’s skincare community, 63% of people who thought they had fungus turned out to have psoriasis. They spent months using antifungal creams that did nothing. Some even got worse. One person wrote: “After 8 months of antifungals, my nail separated and it hurt to touch.” The reverse happens too. People with fungal infections get told they have psoriasis and are given steroid creams or injections. That makes the nail even more brittle and prone to crumbling. The economic cost? In the U.S. alone, misdiagnosis leads to $850 million in wasted spending each year. That’s prescriptions, doctor visits, and tests that didn’t fix the problem.
How Doctors Actually Diagnose These
If you’re seeing a dermatologist, they won’t just guess. They follow a clear path:- Clinical exam: They look for pitting, oil spots, salmon patches-classic psoriasis signs. They check if multiple nails are affected and whether the problem started suddenly or slowly.
- KOH test: A tiny scraping of the nail is mixed with potassium hydroxide and looked at under a microscope. It kills human cells and leaves fungal ones visible. This test is 70-80% accurate and costs $15 to $25.
- Fungal culture or PAS stain: If the KOH is negative but suspicion remains, they send a sample to a lab. Fungal cultures take weeks but are 95% specific. PAS staining is faster and 90% sensitive-it shows fungal threads in the nail tissue.
Some clinics now use reflectance confocal microscopy-a non-invasive imaging tool that can spot psoriasis and fungal patterns in the nail with 92% accuracy. It’s not everywhere yet, but it’s coming.
What Works for Treatment
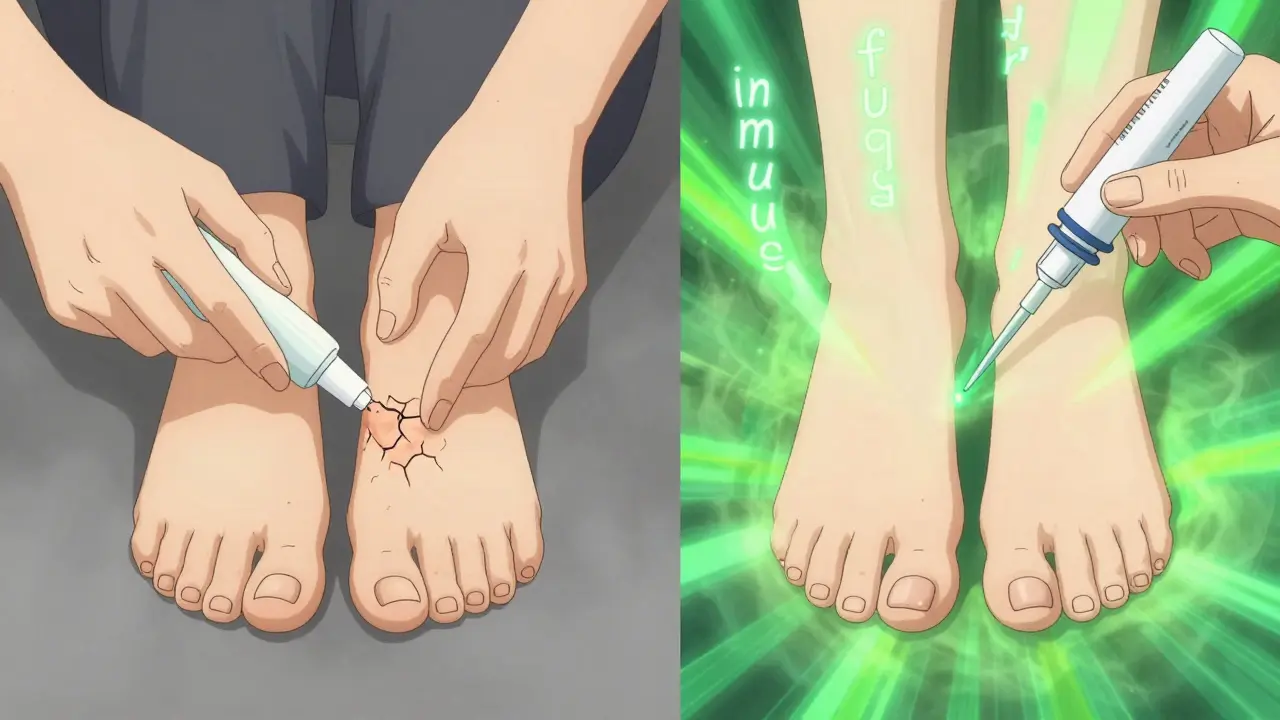
Treatment depends entirely on what you actually have.For fungal infections:
- Oral terbinafine: The gold standard. Taken daily for 12 weeks for toenails, 6 weeks for fingernails. Clears the infection in 78% of cases, confirmed by culture.
- Topical antifungals: Like efinaconazole (Jublia) or ciclopirox. They work, but only if you apply them daily for 9 to 12 months. That’s because nails grow super slow-just 0.1mm per day.
- Home care: Keep nails dry. Humidity above 40% helps fungi grow. Wear open shoes. Change socks daily. Don’t share nail clippers.
For nail psoriasis:
- Corticosteroid injections: Injected right under the nail. Can show improvement in 8 to 12 weeks.
- Biologics: Drugs like secukinumab (Cosentyx) or ixekizumab. These target the immune system. In a 2022 survey, 65% of patients saw major improvement after 24 weeks.
- Topical treatments: Calcipotriol or tazarotene creams, sometimes under occlusion. Help reduce scaling and thickening.
- Home care: Avoid trauma. Don’t pick at nails. Use emollients to keep the skin around the nail soft. Moisturize daily.
And here’s something most people don’t know: nail psoriasis can make fungal infections worse. When the nail bed is inflamed from psoriasis, it’s easier for fungi to invade. About 5% to 30% of psoriasis patients end up with a secondary fungal infection. That’s why treating both at once might be necessary.
What You Can Do at Home
You can’t diagnose yourself, but you can track things better:- Take monthly photos of your nails under the same light. Use a white background. Note any changes in color, thickness, or separation.
- Keep a journal: Did your nail change after you cut it too short? Did it flare after stress? That’s the Koebner phenomenon-trauma triggering psoriasis.
- Don’t use over-the-counter antifungal products if you have psoriasis. They won’t help and may irritate the skin.
- If you have psoriasis on your skin, tell your dermatologist about any nail changes. Don’t wait.
The Future Is Getting Better
New research is changing how we see nail disorders. Scientists at Mount Sinai are studying the nail bed microbiome. They found psoriasis nails have more Staphylococcus bacteria and less Cutibacterium. Fungal nails? Higher levels of Trichophyton DNA. That could lead to a simple swab test that tells you exactly what you have. AI tools are being trained to analyze nail photos. The Global Psoriasis Atlas predicts misdiagnosis rates will drop 22% by 2027 just from better image recognition. Climate change is making things harder, though. Warmer, wetter weather lets fungi spread more easily. The International Society for Human and Animal Mycology expects fungal nail infections to rise 15% in the next decade.Bottom Line
Don’t assume your weird nail is fungus. If you’ve had psoriasis before, it’s probably not. If your nail smells bad and is thickening from the tip, it’s likely fungal. But the only way to know for sure is to get the right tests.Go to a dermatologist-not a general doctor, not a podiatrist unless they specialize in skin. Bring your photos. Tell them your history. Demand a KOH test if they don’t offer one.
Getting the diagnosis right isn’t just about saving money. It’s about stopping the cycle of frustration, pain, and wasted months. Your nails are a window into your health. Pay attention to them.
Can nail psoriasis turn into a fungal infection?
Yes. Nail psoriasis damages the nail bed and creates cracks or separation, which lets fungi slip in. About 5% to 30% of people with nail psoriasis develop a secondary fungal infection. That’s why treating the psoriasis first is important-it reduces the risk.
Do antifungal creams work for nail psoriasis?
No. Antifungal creams target fungi, not autoimmune reactions. Using them on psoriasis won’t help and can irritate the skin, making the condition worse. If you’ve tried antifungals and your nails got worse, it’s a red flag you might have psoriasis.
How long does it take to see results from psoriasis nail treatment?
It depends. Corticosteroid injections can show improvement in 8 to 12 weeks. Biologics like secukinumab take about 24 weeks for full results because nails grow slowly. Patience is key-you’re waiting for the damaged nail to grow out and be replaced.
Is nail psoriasis contagious?
No. Nail psoriasis is an autoimmune condition, not an infection. You can’t catch it from someone else. But if you have psoriasis, you’re more likely to get a fungal infection, which is contagious. Keep your nails clean and dry to reduce that risk.
Can I treat both conditions at the same time?
Yes, if you have both. A dermatologist can prescribe an oral antifungal like terbinafine while also starting a biologic for psoriasis. Treating the psoriasis helps prevent future fungal invasions. Don’t try to manage both on your own-this requires professional coordination.
Why do my nails keep coming back after treatment?
Fungal infections can return if you’re exposed again-like walking barefoot in gyms or pools. Psoriasis can flare due to stress, injury, or illness. For both, recurrence is common. The key is ongoing management: keep nails trimmed, avoid trauma, monitor for early signs, and don’t ignore changes.


Comments
Lily Steele January 30, 2026 AT 20:05
My nails have been weird for years and I thought it was fungus. Turns out it was psoriasis. I wasted $300 on antifungal stuff that did absolutely nothing. Finally saw a derm who did a KOH test and boom - turned out to be nail psoriasis. Started injections and now my nails look normal again. Don’t let anyone tell you it’s just fungus if you’ve got skin psoriasis.
Rohit Kumar January 30, 2026 AT 23:44
Reading this feels like someone finally explained what’s been happening to my nails for 8 years. I’ve been told it’s fungus, then psoriasis, then just aging. No one ever mentioned pitting. I didn’t even know that was a thing. Now I’m going back to my derm with this post printed out. Thank you.
Beth Beltway January 31, 2026 AT 01:56
Wow. Another person who doesn’t understand basic medical science. You can’t just ‘look’ at a nail and diagnose psoriasis vs fungus. That’s dangerous pseudoscience. You need lab confirmation. Period. This post is misleading people into skipping tests. Don’t be a DIY doctor.
kate jones January 31, 2026 AT 19:54
Actually, Beth, she’s not wrong. The clinical signs are so distinct when you know what to look for. KOH is a screening tool, not a gold standard - false negatives are common. PAS staining and confocal microscopy are far more reliable. The 52% misdiagnosis rate in primary care? That’s not because people are guessing - it’s because they’re not trained to recognize the subtle signs like salmon patches or pitting. This post is accurate, evidence-based, and desperately needed.
Kelly Weinhold February 2, 2026 AT 13:03
Okay but can we just take a second to appreciate how much this post helped me? I’ve been so ashamed of my nails for years - thought I was gross, like I didn’t wash my hands or something. Turns out it’s not my fault, it’s my immune system being weird. And now I know I can actually fix it? I’m not just stuck with this? I cried reading this. Thank you so much for writing it.
Kimberly Reker February 2, 2026 AT 18:29
I’ve had psoriasis since I was 12. My nails were the last thing I ever talked about. Too embarrassing. Now I’m 34 and finally got the right diagnosis after 22 years. Biologics changed my life. My nails are growing back clean. If you’re reading this and you’ve got psoriasis - don’t wait. Tell your derm about your nails. They’re not just cosmetic. They’re a signal.
Blair Kelly February 4, 2026 AT 14:12
Let’s be real - 90% of people who think they have fungus don’t even know what a KOH test is. They buy OTC creams from the drugstore and rub them on for six months while their nail turns black and crumbles. Meanwhile, their psoriasis is silently raging. This isn’t just a nail problem - it’s a systemic failure in primary care. We need mandatory dermatology training for GPs. And if you’re a doctor reading this: if a patient has skin psoriasis and nail changes - STOP ASSUMING FUNGUS. Run the test. Or refer them. You’re costing people years of their life.
owori patrick February 6, 2026 AT 01:37
In Nigeria, most people just go to the market and buy herbal creams. They don’t even know what a dermatologist is. I’ve seen nails turn black and fall off because no one knew the difference. This post should be translated into pidgin and shared in every village. Nail health is invisible health - until it’s not.
Carolyn Whitehead February 8, 2026 AT 01:00
I just looked at my thumb and there’s a little pit. I think I might have psoriasis. I’m scared to tell my doctor because I don’t want to be labeled. But maybe I should just say something. I don’t know.
Marc Bains February 9, 2026 AT 01:52
Kelly, you’re not alone. I was scared too. I waited three years before I said anything. Then I walked in and said, ‘I think my nails are psoriasis.’ My derm didn’t blink. She just said, ‘Let’s check.’ Five minutes later, she pointed out the pitting I’d been ignoring for years. You don’t have to be ‘the problem’ to get help. You’re just someone who noticed something. That’s enough.