Most people don’t realize pancreatic cancer often shows no clear signs until it’s advanced. By the time symptoms appear, the cancer has usually spread. That’s why survival rates stay so low - only 12% of patients live five years after diagnosis. But that’s changing. New research is uncovering earlier warning signs, and treatments are getting smarter, more targeted, and more effective than ever before.
What You Might Miss: The Silent Symptoms
Pancreatic cancer doesn’t scream for attention. It whispers. And too often, those whispers get ignored.Abdominal or back pain is one of the most common early signs, reported by 65 to 75% of patients. It’s often described as a dull, constant ache that doesn’t go away with rest or painkillers. Many mistake it for something less serious - like a pulled muscle, gallstones, or even stress.
Unexplained weight loss is another red flag. If you’re eating normally but dropping pounds without trying, it’s not just bad luck. Around 60% of people diagnosed with pancreatic cancer lose significant weight before they even get a diagnosis. This isn’t about dieting. It’s the tumor disrupting digestion and metabolism.
Jaundice is harder to ignore. Yellowing of the skin and eyes, dark urine, and pale, greasy stools are classic signs - especially if the tumor is in the head of the pancreas, blocking the bile duct. You might also feel intense itching, even without a rash. These symptoms happen because bile can’t flow normally, and bilirubin builds up in the blood. Levels above 2.5 mg/dL are a clear signal.
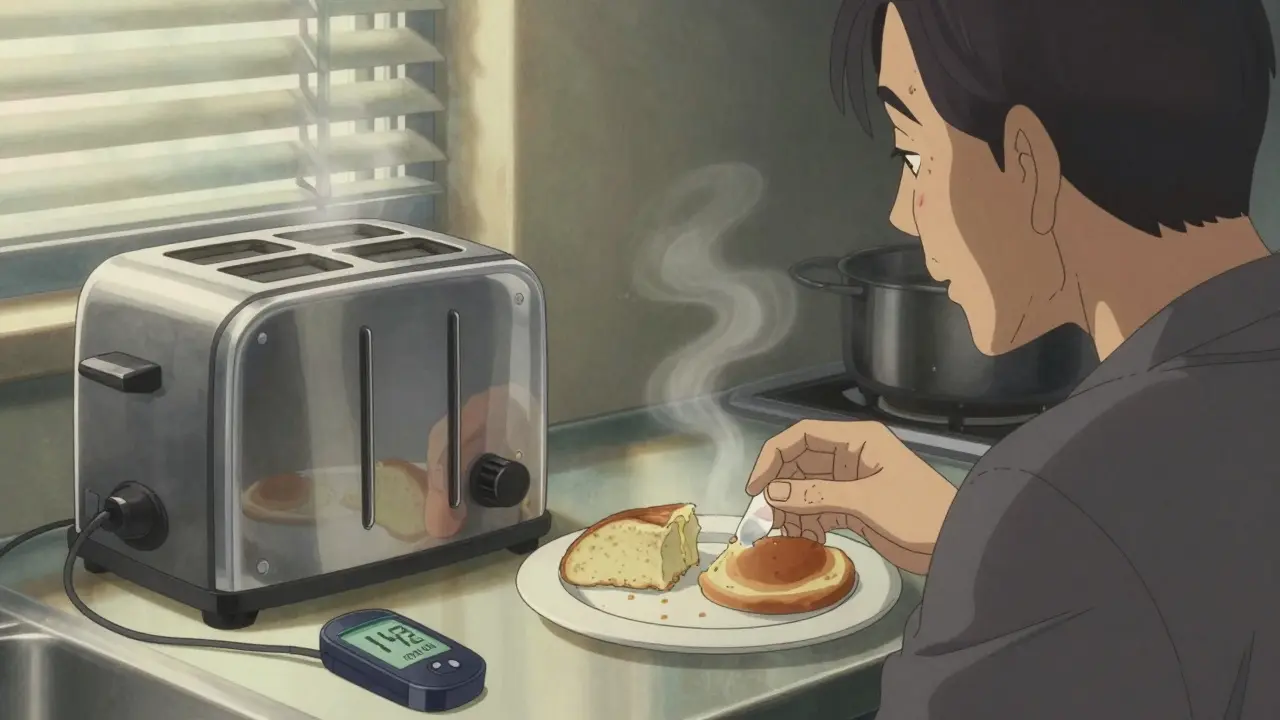
Then there’s new-onset diabetes. This is one of the most overlooked clues. About 80% of people with pancreatic cancer develop diabetes within 18 months of their cancer diagnosis. Their blood sugar spikes - from normal (under 100 mg/dL) to diabetic levels (over 126 mg/dL) - often within just six months. If you’ve never had diabetes before and suddenly need medication, ask your doctor: could this be a sign of something else?
Depression and anxiety can show up months before physical symptoms. A 2018 study found that nearly half of pancreatic cancer patients experienced major mood changes as their first symptom. It’s not just emotional stress. The tumor releases chemicals that affect brain chemistry. If you’re feeling persistently low, hopeless, or anxious - and there’s no clear reason why - it’s worth mentioning to your doctor.
Why Diagnosis Is So Hard
The pancreas is tucked deep behind the stomach, hidden from routine exams. You can’t feel a tumor with your hands. No simple blood test catches it early. Even CT scans miss small tumors - only 60% of tumors under 2 cm show up clearly.CA 19-9 is the most common blood marker used, but it’s unreliable for early detection. It’s elevated in only 30-50% of early-stage cases. By the time it’s high, the cancer is often already advanced.
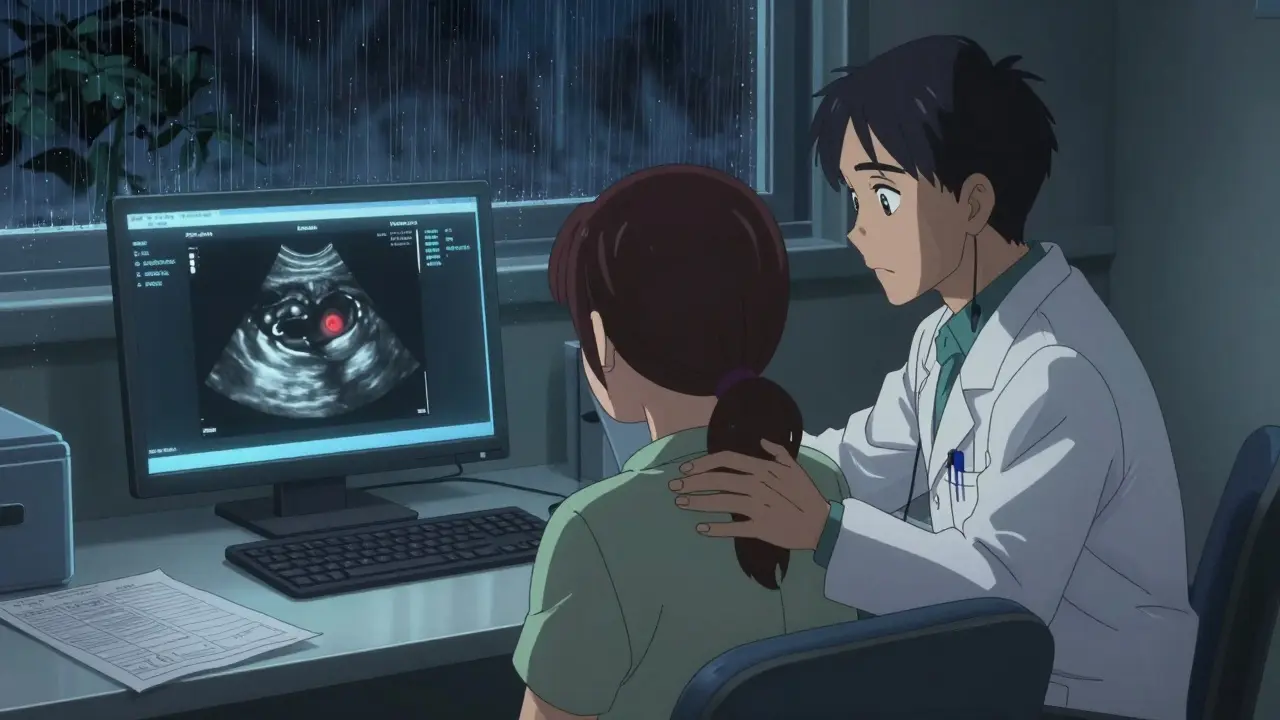
That’s why diagnosis usually requires a mix of tools: imaging (CT or MRI), blood tests, and a biopsy. The most accurate way to get tissue is through endoscopic ultrasound (EUS), where a thin tube with a camera is passed through the mouth to the pancreas. A tiny needle pulls out cells for analysis. This method is 95% accurate when done right.
But here’s the problem: most people don’t get tested until they’re already sick. Only 20% of pancreatic cancers are found early enough for surgery. The rest are diagnosed at stage III or IV, when the cancer has spread to nearby organs or distant sites like the liver.
What’s Changed in Treatment
Ten years ago, a diagnosis of advanced pancreatic cancer meant months, not years. Today, survival is improving - slowly, but significantly.Surgery is still the only chance for a cure. The Whipple procedure removes part of the pancreas, the gallbladder, part of the small intestine, and sometimes part of the stomach. For early-stage patients, 5-year survival jumps to 20-25%. But only 15-20% of patients are even eligible for surgery when first diagnosed.
That’s why neoadjuvant therapy - treatment before surgery - is becoming standard. Chemotherapy like FOLFIRINOX (a mix of four drugs) shrinks tumors in 58% of borderline resectable cases. That means more people who were told “no surgery” now get a second chance.
For those with metastatic disease, the game-changer was the PRODIGE 24 trial. Patients on modified FOLFIRINOX lived an average of 54.4 months - more than four and a half years - compared to just 20.2 months with older treatments. That’s not a cure, but it’s life-changing.
Targeted therapies are making a difference for specific genetic groups. If you have a BRCA gene mutation (often linked to breast and ovarian cancer), the drug olaparib can slow cancer progression by over seven months. For the rare 3-4% of patients with MSI-H/dMMR tumors, immunotherapy like pembrolizumab can trigger strong, lasting responses.
Genetic testing is no longer optional. If you’re diagnosed, ask for it. Knowing your tumor’s DNA helps your doctor pick the best drugs - and might even help your family members understand their own risk.
Early Detection Is the New Frontier
The real hope lies in catching pancreatic cancer before it spreads.Right now, only high-risk people get screened: those with inherited syndromes like BRCA mutations, Lynch syndrome, or hereditary pancreatitis. They’re offered annual MRI or endoscopic ultrasound starting at age 50.
But new tools are emerging. Johns Hopkins developed PancreaSeq, a test that detects cancer DNA in pancreatic fluid with 95% accuracy in high-risk groups. The DETECTA trial is testing a blood test that looks for tumor DNA and protein markers - it’s already showing 85% accuracy in early results.
Even AI is stepping in. Google Health’s LYNA algorithm can spot cancer cells in tissue slides with 99.3% accuracy. It’s not in clinics yet, but it’s a sign of what’s coming.
And then there’s the connection with diabetes. Doctors are now watching people who develop diabetes after age 50, especially if they’re not overweight or don’t have a family history. That group is being studied as a potential early-warning population.
What You Can Do Now
There’s no magic bullet. But you can take steps to protect yourself.- If you’ve had unexplained weight loss, new abdominal pain, or jaundice - don’t wait. See a doctor.
- If you’re newly diagnosed with diabetes after 50, ask about pancreatic cancer screening - especially if you have other risk factors.
- If you have a family history of pancreatic, breast, ovarian, or colon cancer, talk to a genetic counselor.
- Don’t ignore depression or anxiety that comes out of nowhere. It could be your body’s first signal.
Survival rates are rising because we’re catching more cases earlier and treating them better. The 5-year survival rate for localized tumors is now 44%. That’s not just a number - it’s a reason to act.
Can pancreatic cancer be detected with a routine blood test?
No, there’s no standard blood test for early detection. The CA 19-9 marker is sometimes used, but it’s not reliable until the cancer is advanced. It misses up to 70% of early-stage tumors. New blood tests that look for tumor DNA and protein markers are in trials and show promise, but they’re not yet available for general use.
Is pancreatic cancer hereditary?
About 10% of pancreatic cancers are linked to inherited gene mutations. BRCA1, BRCA2, Lynch syndrome, and hereditary pancreatitis are the most common. If you have two or more close relatives with pancreatic cancer, or if you have a known mutation, genetic testing and regular screening may be recommended.
Why is jaundice a key symptom?
Jaundice happens when a tumor in the head of the pancreas blocks the bile duct. Bile builds up in the blood, turning skin and eyes yellow. Dark urine and pale stools are direct results - urine gets dark from excess bilirubin, and stools turn pale because bile isn’t reaching the intestines. These are clear, measurable signs that need immediate evaluation.
Can lifestyle changes prevent pancreatic cancer?
You can’t prevent it completely, but you can lower your risk. Smoking doubles your risk - quitting helps. Obesity and chronic pancreatitis also raise risk. Eating a balanced diet, staying active, and avoiding heavy alcohol use can reduce your chances. But even healthy people get it - which is why early symptoms matter more than prevention.
What’s the survival rate if caught early?
If pancreatic cancer is found before it spreads - called localized stage - the 5-year survival rate is 44%. That’s a big jump from the overall 12%. Surgery is possible at this stage, and outcomes are much better. That’s why recognizing early symptoms like new-onset diabetes, unexplained weight loss, or jaundice can save lives.
Are there any new treatments on the horizon?
Yes. Liquid biopsies that detect mutant KRAS in blood are being tested and could revolutionize early detection within the next five years. AI tools are improving how we read scans and tissue samples. New drug combinations are being tested in clinical trials, especially for tumors with rare mutations. The goal is personalized treatment - matching each patient’s tumor profile to the most effective therapy.

Comments
Rosalee Vanness January 14, 2026 AT 02:23
God, I wish I’d known about the depression link sooner. My aunt went from being this vibrant, joke-telling force of nature to this hollow shell over six months - no weight loss, no jaundice, just... sadness. She thought it was grief from her mom passing, but it was the tumor whispering. I keep thinking if we’d pushed for an ultrasound when she said she felt "off" inside, maybe...
Now I tell everyone I know: if your mood drops outta nowhere and nothing in your life explains it, don’t brush it off. It’s not just stress. It’s your body screaming in a language most doctors don’t speak yet.
mike swinchoski January 15, 2026 AT 03:02
Why do people keep acting like this is some big secret? It’s just cancer. You eat bad, you get sick. Stop overcomplicating it. If you’re fat and lazy, you get pancreatic cancer. That’s it.
Angel Tiestos lopez January 16, 2026 AT 20:45
Brooo… this hit different 😔
I used to think cancer was just "bad luck" - like getting struck by lightning. But now? It’s like your body’s sending smoke signals and we’re all too busy scrolling to notice. New diabetes after 50? Not a snack problem - it’s a red flag waving in your pancreas’s last breath.
And depression? That ain’t just "feeling down." That’s your tumor doing a rave in your brain with no invite. We gotta start listening to the quiet ones - even if they don’t yell.
Also, if you’re still using CA 19-9 like it’s a crystal ball… we got work to do 🙏
Acacia Hendrix January 18, 2026 AT 14:21
It’s fascinating how the literature still treats CA 19-9 as a diagnostic pillar when its sensitivity in early-stage disease hovers around 30–50%. The real paradigm shift lies in multi-omic biomarker panels - specifically, those integrating ctDNA methylation signatures with proteomic profiles of exosomal CD63+ vesicles.
Until we move beyond crude tumor markers and embrace liquid biopsy platforms validated in prospective cohorts like the DETECTA trial, we’re merely rearranging deck chairs on the Titanic of late-stage detection.
James Castner January 18, 2026 AT 20:53
Let me be clear: this is not just a medical issue - it’s a societal failure. We have the tools. We have the science. We have the data. Yet, we continue to treat pancreatic cancer like a ghost story - something that whispers, and we pretend not to hear.
When a 58-year-old woman develops diabetes out of nowhere, we give her metformin. We don’t order an EUS. When a man complains of back pain and says "it’s just stress," we send him to a chiropractor. We don’t scan his pancreas.
This isn’t about innovation. It’s about urgency. It’s about seeing people - not just symptoms. We owe it to the 12% who don’t make it to five years to stop waiting for the scream. The whisper is enough. Listen.
And if you’re reading this and you’re a doctor - change your practice. If you’re a patient - demand more. If you’re a family member - don’t let silence be the diagnosis.
Adam Rivera January 19, 2026 AT 01:33
My uncle was diagnosed at stage 4. He didn’t even know he was sick until he turned yellow. But man - he lived 3 years on modified FOLFIRINOX. Three years of fishing, grandkids’ birthdays, Sunday pancakes. That’s not just a statistic - that’s a miracle we didn’t have 10 years ago.
So yeah, the odds are rough. But we’re bending the curve. And if you’re reading this because you’re scared? You’re already doing something right. Knowledge is power. Keep asking questions. Keep pushing. We’re getting better.
Damario Brown January 20, 2026 AT 15:45
Wow, another cancer post full of feel-good nonsense. Let me guess - you think if you "listen to your body" you’ll avoid death? Newsflash: cancer doesn’t care if you’re woke or woke enough. CA 19-9 is garbage. EUS is invasive. FOLFIRINOX kills people faster than the disease. You’re all just chasing hope like it’s a TikTok trend.
And don’t even get me started on the "new diabetes = cancer" myth. I’ve seen 20 diabetics. Only one had pancreatic cancer. That’s 5%. You’re scaring people for clicks.
Priyanka Kumari January 21, 2026 AT 12:47
This is so important. In India, many people still think cancer is punishment or fate. But this article? It’s a wake-up call. My cousin had unexplained weight loss and was told she had "digestive issues." Two years later - stage 4. If we had known about the diabetes link, maybe…
Now I share this with every auntie and uncle who says "don’t worry, it’s just gas." We need to change the culture of silence. Knowledge saves lives. Thank you for writing this.
Avneet Singh January 22, 2026 AT 06:56
Typical Western medical hubris. You treat symptoms like puzzles to be solved with $50,000 scans and targeted therapies, but ignore root causes: processed food, sedentary lifestyles, chronic inflammation. All this talk of FOLFIRINOX and olaparib? It’s just profit-driven palliative care dressed up as innovation. Real prevention? Eat real food. Move. Sleep. Stop chasing tech solutions to lifestyle failures.
vishnu priyanka January 23, 2026 AT 08:42
Man, I read this at 2am after my dad’s last chemo. He’s still here. Not cured, but here. And you know what? The weirdest thing? He started getting really moody six months before the pain started. We thought he was just tired of being old.
Turns out, his pancreas was throwing a silent party inside him. This article? It’s like someone finally translated his body’s secret language.
Thanks for writing this. I’m printing it out for my whole family.
Alan Lin January 24, 2026 AT 08:17
I want to respond to the comment about CA 19-9 being unreliable - and I agree. But let’s not dismiss it entirely. It’s not a diagnostic tool, but it’s a vital monitoring tool. For patients undergoing neoadjuvant therapy, a declining CA 19-9 trend correlates strongly with tumor response - even when imaging is ambiguous.
And for those asking about genetic testing: if you have a BRCA mutation, your siblings and children need to know. This isn’t just about you. It’s about your lineage. Genetic counseling isn’t optional - it’s preventative medicine for future generations.
To the person who said "it’s just cancer" - this isn’t about blame. It’s about awareness. And awareness, in this case, is the only thing standing between a diagnosis and a death sentence.
Robin Williams January 24, 2026 AT 10:08
Wait… so if I get diabetes after 50 and I’m skinny? That’s not me eating too much sugar… it’s my pancreas screaming for help? 🤯
I just got my A1C back - 6.2. I thought I was just getting older. Now I’m booking an EUS. Not because I’m scared… but because I’m done ignoring whispers.
Scottie Baker January 24, 2026 AT 20:05
Y’all are overthinking this. If your skin’s yellow and you’re losing weight? Go to the ER. Don’t read Reddit. Don’t wait for AI. Just go. I’ve seen it. It’s not pretty. But it’s faster if you don’t waste time.