When you pick up a prescription, do you check the label? Not for the name of the drug - but for the company that made it. If it’s not the brand you remember, you might feel uneasy. That’s not just about price. It’s about brand psychology. And it’s one of the biggest hidden barriers to generic medication use - even when those pills work just as well.
Why Patients Doubt Generics - Even When They Work
You’ve probably heard it: "Generic drugs are identical to brand-name ones." And technically, that’s true. The FDA and EMA require generics to have the same active ingredient, strength, dosage form, and bioequivalence - meaning they deliver the same amount of medicine into your bloodstream within the same time frame. The difference? The color, shape, packaging, and price. But here’s the catch: patients don’t always believe it. A 2024 study in Nature Communications found that 72% of patients reported dissatisfaction with at least one generic medication they’d been switched to. Why? Not because the drug failed. But because they felt it didn’t work. One patient wrote on Reddit: "Switched from Synthroid to generic levothyroxine - my TSH levels went wild." Another said: "Generic statins just don’t lower my cholesterol like the brand did." The truth? In most cases, the medication is the same. But the mind doesn’t care about bioequivalence studies. It cares about experience, memory, and trust. If you’ve been on a brand-name pill for years - say, Lipitor - and your doctor suddenly hands you a little white tablet labeled "atorvastatin," your brain doesn’t see "same drug." It sees "cheaper," "unknown," and maybe even "inferior." This isn’t irrational. It’s human.What Actually Drives Patient Satisfaction With Generics?
Researchers have built tools to measure this. One of the most widely used is the Generic Drug Satisfaction Questionnaire (GDSQ), a 12-item survey that breaks satisfaction into three parts: effectiveness, convenience, and side effects. The results? Effectiveness matters most - but not because generics are less effective. It’s because patients perceive them as less effective. A 2021 path analysis showed that perceived effectiveness had a stronger impact on satisfaction than actual clinical outcomes. In fact, the study found that if a patient believed a generic was less effective - even if lab results showed no difference - their satisfaction dropped by 37%. Convenience came second. If you had to pick up your meds from a different pharmacy, or if the pill looked completely different, satisfaction fell. Side effects? Third. But even here, patients blamed the generic for side effects they’d always had - just never noticed before. Here’s the kicker: the same pill, taken by two people, can trigger two completely different experiences - not because of the drug, but because of what they believe about it.Who Trusts Generics - And Who Doesn’t?
Not everyone doubts generics. In fact, many people love them. A 2023 study in Saudi Arabia found that 63.8% of satisfied users cited cost savings as the main reason they stuck with generics. "I couldn’t afford my insulin every month until I switched," one patient said. "Now I take it without skipping doses." But trust isn’t evenly distributed. Older adults (over 60) and employed people show higher acceptance rates - 71.4% and 82.1% respectively - according to a 2024 Greek study. Why? Older patients have more experience with the healthcare system. Employed people are more likely to have insurance that pushes generics, and they’ve had time to test them out. On the flip side, younger patients, especially those managing chronic conditions like epilepsy or depression, are far more skeptical. Antiepileptic generics had only 68.9% satisfaction in one 2023 study. Antidepressants? Even worse. Reddit threads are full of stories like: "Generic sertraline made me feel like a zombie. Switched back to Zoloft - instant difference." But here’s what those stories don’t tell you: in double-blind trials, patients can’t tell the difference between brand and generic antidepressants. Yet in real life, when they know they’re on a generic, they report worse side effects. That’s the power of expectation.
Doctors and Pharmacists Are the Missing Link
The biggest factor influencing whether a patient accepts a generic? The person handing them the prescription. Professor Dimitrios T. Boumpas from the University of Athens put it plainly: "Healthcare providers serve as the primary information source about generics for patients." When a doctor says, "This generic is exactly the same," and explains why - with real data, not just a hand wave - satisfaction jumps. A 2023 PLOS ONE study showed a 34.2% increase in patient satisfaction when providers explained the FDA’s 80-125% bioequivalence range. Pharmacists matter too. If the pharmacist says, "This is the same medicine, just cheaper," and takes a minute to answer questions, patients feel heard. But if they just hand over the bottle and say, "It’s generic," patients feel dismissed. In Europe, where pharmacists are more involved in patient education, satisfaction scores are 12.4% higher than in the U.S. for complex generics like anticoagulants and seizure meds. It’s not the drug. It’s the conversation.Why This Matters Beyond Feelings
This isn’t just about comfort. It’s about survival. Non-adherence to medication costs the U.S. healthcare system $300 billion a year. That’s not because people are lazy. It’s because they stop taking their pills - often because they don’t trust them. A patient who thinks their generic blood pressure pill isn’t working might skip doses. Or stop entirely. Then they end up in the ER. Or worse. Each 10% increase in patient satisfaction with generics leads to a 6.3% rise in generic dispensing rates. That’s not just good for wallets - it’s good for public health. Generics make up 90.7% of all prescriptions in the U.S. But they account for only 22.8% of drug spending. That’s a massive savings - if people actually use them.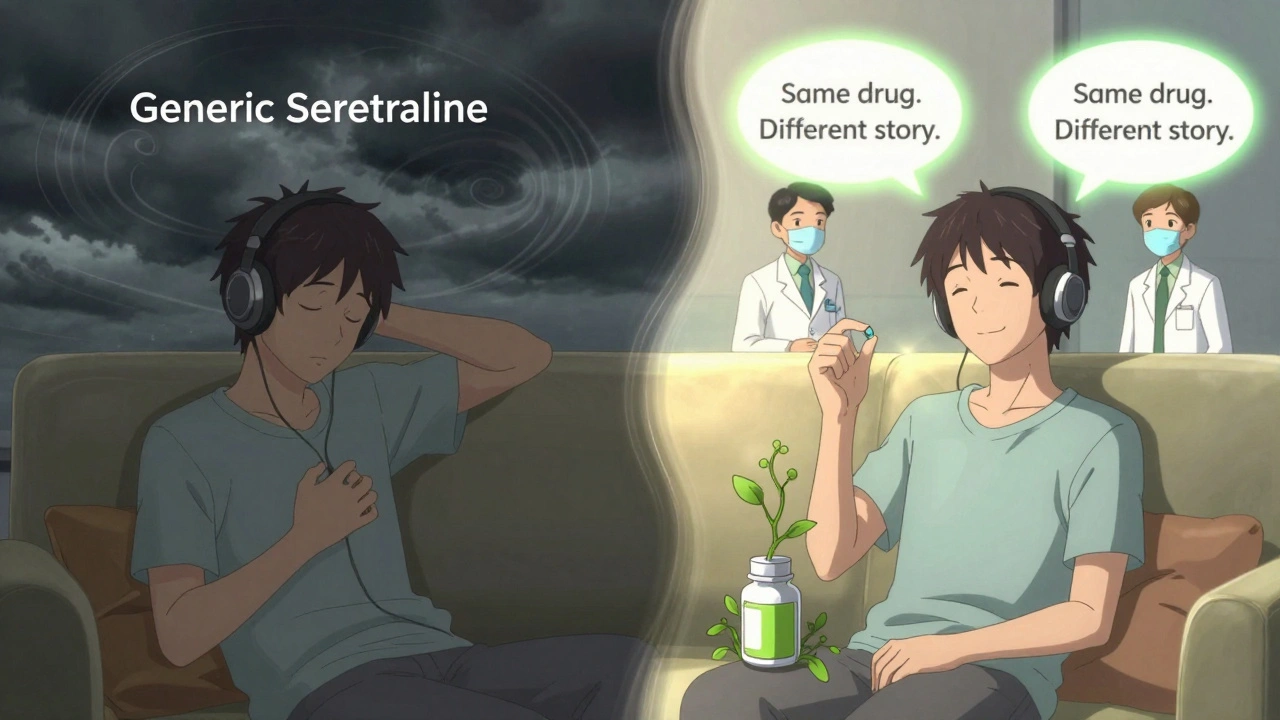
What’s Changing - And What’s Next
The FDA just launched its Generic Drug User Fee Amendments (GDUFA) III Patient Perception Initiative - a $15.7 million project to build better ways to measure satisfaction. They’re using AI to scan 500,000 social media posts across 28 languages to understand how people really talk about generics. Are they angry? Confused? Grateful? Meanwhile, the Mayo Clinic is testing something new: pharmacogenomic satisfaction assessments. Instead of asking, "Do you trust this pill?" they’re asking, "Does your body respond to this version?" By linking genetic markers to how patients metabolize drugs, they’re predicting who’s likely to feel a difference - even if it’s just psychological. Early results show 28.7% better accuracy in predicting satisfaction than old-school surveys. And in the UK, NHS pharmacies are starting to offer "medication reviews" - free 15-minute chats where patients can ask, "Why did they switch me?" and get real answers. Early data shows a 27% drop in complaints about generics after these sessions.Bottom Line: It’s Not the Pill. It’s the Perception.
Generics aren’t inferior. They’re not risky. They’re not second-rate. They’re the same medicine, sold at a fraction of the cost. But until we fix the story people tell themselves about them - until we stop treating patients like passive recipients and start treating them like partners - satisfaction will stay stuck. The fix? Simple. Talk. Explain. Listen. Don’t just hand over a pill. Hand over confidence.If you’ve been switched to a generic and feel something’s off - tell your doctor. Don’t assume it’s the drug. Ask: "Could this be my mind playing tricks?" Sometimes, it is. And that’s okay. The right conversation can make all the difference.


Comments
Richard Ayres December 13, 2025 AT 06:28
It's fascinating how much psychology plays into medication adherence. I've seen patients refuse generics outright, even when they can't afford the brand, simply because they believe the pill 'looks wrong.' The real tragedy is that this isn't about ignorance-it's about trust, and we as providers often fail to build it. A simple five-minute conversation about bioequivalence can turn a skeptic into a believer. We need more of that, not less.
It’s not just about the drug. It’s about the ritual-the color, the shape, the bottle. We’ve conditioned people to equate appearance with efficacy. That’s a cultural artifact we need to reprogram.
Karen Mccullouch December 14, 2025 AT 14:30
Ugh, I HATE when they switch me to generics! 😤 My blood pressure was PERFECT on Lisinopril HCTZ brand, then they gave me some white pill with a weird logo and now I’m dizzy all day. It’s NOT the same! Who cares what the FDA says-MY BODY KNOWS THE DIFFERENCE. 🤬
They’re just trying to save money while I pay with my health. Screw this system.
Himmat Singh December 16, 2025 AT 11:04
One must acknowledge the empirical veracity of the bioequivalence standards promulgated by regulatory authorities; however, the phenomenological experience of the patient, though non-quantifiable, remains a valid construct within the hermeneutics of medical anthropology. The disjunction between objective pharmacokinetics and subjective therapeutic perception constitutes a hermeneutic gap that cannot be bridged by statistical data alone.
It is, therefore, imperative that the epistemological framework of modern pharmacology evolve to incorporate patient narrative as a primary data stream, rather than an anecdotal outlier. To dismiss perception as mere placebo is to commit the fallacy of scientism.
kevin moranga December 16, 2025 AT 23:11
Hey, I get it. I used to be super skeptical about generics too-until I tried one for my cholesterol and saved $80 a month. I was nervous, but I tracked my labs for three months. Nothing changed. Same numbers, same energy, same sleep. Turns out my brain was the problem, not the pill.
Here’s the thing: if you’re feeling off after a switch, don’t just assume it’s the drug. Talk to your doc. Ask them to check your levels. Sometimes it’s just your mind playing tricks. Other times, it’s a formulation issue-rare, but it happens. Either way, don’t quit. Just dig a little deeper. You’ve got this.
And if you’re a provider? Don’t just hand over the bottle. Say, ‘Hey, I know this looks different, but here’s why it’s the same-and here’s how we’ll know it’s working for YOU.’ That kind of care? It changes lives.
Alvin Montanez December 17, 2025 AT 22:51
Let’s be brutally honest: people who complain about generics are either lazy, entitled, or both. You think your body is so special that it can tell the difference between a $2 pill and a $120 pill? The FDA doesn’t approve generics based on wishful thinking-they test them. Repeatedly. In double-blind trials. With thousands of patients.
And yet, people still cling to brand names like some kind of placebo talisman. This isn’t science. It’s superstition dressed up as health advocacy. If you’re too weak to handle a different-colored pill, maybe you shouldn’t be managing your own meds.
Stop letting marketing and fear dictate your health decisions. The system isn’t broken. You are.
Lara Tobin December 18, 2025 AT 07:38
I had a friend who switched from Zoloft to generic sertraline and cried for a week saying she felt ‘numb and hollow.’ She thought she was failing. But she didn’t tell her doctor-she just stopped. I sat with her for hours and said, ‘What if it’s not the pill? What if it’s the fear?’
She went back, talked to her pharmacist, got a detailed handout, and slowly realized she’d been scared of the change, not the drug. Two weeks later, she said she felt ‘like herself again.’
It’s not about the pill. It’s about feeling heard. 💙
Jamie Clark December 18, 2025 AT 10:00
The entire premise of this post assumes that ‘perception’ is the problem. But what if perception is the truth? If your body responds differently to a generic, does it matter if the FDA says it’s ‘bioequivalent’? What is ‘equivalence’ if not a statistical abstraction that ignores the lived reality of individual biology?
Pharmacology treats the human body like a machine with interchangeable parts. But we’re not machines. We’re ecosystems shaped by genetics, environment, trauma, belief, memory. A pill isn’t just chemistry-it’s a symbol. And symbols have power.
Maybe the real failure isn’t patient perception. Maybe it’s the medical system’s refusal to acknowledge that meaning matters as much as molecules.
Keasha Trawick December 19, 2025 AT 23:19
Okay, let’s talk about the *vibe* of a pill. 🤯
Brand-name meds? They come in sleek bottles with that signature logo, that crisp label, that *aura* of science and stability. Generic? A little white oval with a code stamped on it like it’s a prison ID. No wonder people feel like they’re being handed leftovers.
And don’t get me started on the color psychology-blue for calm, green for natural, red for potency. Generics? White. Bland. Invisible. Like the pharmaceutical equivalent of beige wallpaper.
Meanwhile, Big Pharma spends billions on branding that makes a pill feel like a magic bullet. And now they’re surprised patients don’t trust the knockoff? Honey, it’s not about efficacy. It’s about *brand equity*. We’ve turned medicine into a luxury good. And generics? They’re the thrift-store version of salvation.