Alfacip: Uses, Dosage, Side Effects & Interactions
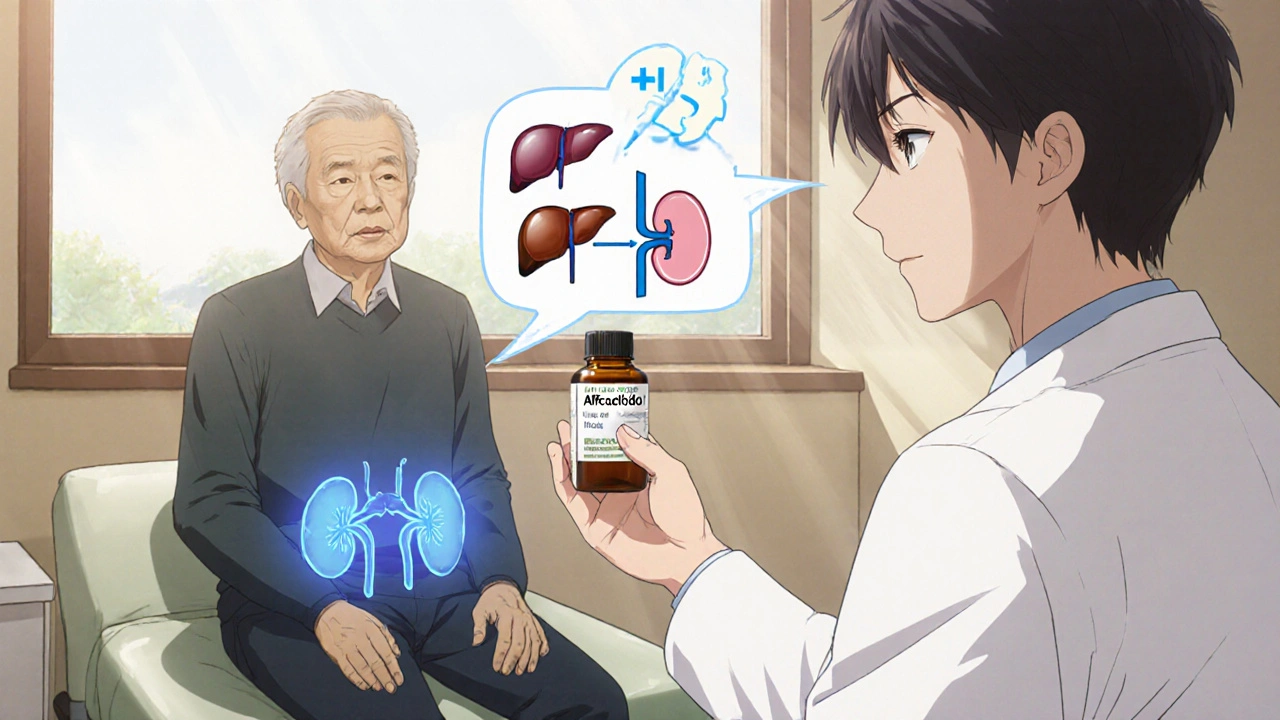
When you see Alfacip, a brand‑name tablet that contains amlodipine, a calcium‑channel blocker prescribed for high blood pressure and chest pain. Also known as Amlodipine Besylate, it works by relaxing the smooth muscle in arterial walls, which lowers hypertension, a chronic elevation of blood‑pressure readings that strains the heart and vessels. This action makes Alfacip a staple in treating cardiovascular disease, any condition affecting the heart or blood vessels, such as angina or heart failure. The drug belongs to the class of calcium channel blockers, medications that block L‑type calcium channels to reduce vascular resistance, and its active ingredient is amlodipine, a long‑acting dihydropyridine that provides steady blood‑pressure control over 24 hours. Because it targets a specific pathway, Alfacip can be combined safely with many other antihypertensives, yet it does have a few caveats. For most adults, the standard starting dose is 5 mg once daily, but doctors may adjust the amount based on age, liver function, or how well the patient responds. The medication is taken with or without food, and consistency in timing helps maintain stable plasma levels. If you miss a dose, the advice is simple: take it as soon as you remember unless it’s almost time for the next one—don’t double up. Understanding these basics sets the stage for deeper insight into dosing nuances, side‑effects, and drug‑interaction warnings that follow.
Alfacip’s dosing flexibility is one of its strengths. While 5 mg works for many, some patients need 10 mg to reach target blood‑pressure goals, especially those with severe hypertension or resistant angina. Elderly patients or those with moderate hepatic impairment often start at 2.5 mg to avoid excessive blood‑pressure drops. The drug’s half‑life of about 30–50 hours means steady effects, but it also means side effects can linger if the dose is too high. Common side effects include swelling of the ankles (peripheral edema), a flushing sensation, and mild headache; these stem from vasodilation and are usually mild and transient. Less frequent issues like dizziness, fatigue, or a rapid heartbeat (tachycardia) should prompt a check‑in with your clinician. Because Alfacip can affect how the heart works, regular monitoring of blood‑pressure readings and, when indicated, an ECG are good practices. Patients with a history of heart failure should be cautious, as the fluid‑retaining effect might exacerbate symptoms. If you notice sudden weight gain, increased shortness of breath, or swelling that doesn’t improve, contact a healthcare professional quickly.
Beyond the typical side‑effects, drug interactions are where vigilance pays off. Alfacip is metabolized mainly by the liver enzyme CYP3A4, so strong inhibitors like ketoconazole, erythromycin, or grapefruit juice can raise amlodipine levels and increase the risk of low blood pressure or edema. Conversely, strong inducers such as rifampin or carbamazepine may lower drug concentrations, making the medication less effective. Combining Alfacip with other blood‑pressure agents—especially other calcium‑channel blockers, ACE inhibitors, or ARBs—usually improves control but may amplify the drop in blood pressure, so dose adjustments are common. For patients on statins like simvastatin, a modest dose reduction of the statin is recommended because amlodipine can increase statin levels, raising the chance of muscle pain. Pregnant or breastfeeding women should avoid Alfacip unless the benefit clearly outweighs the risk, as safety data are limited. With these considerations in mind, you’ll be better equipped to manage therapy, avoid pitfalls, and enjoy the blood‑pressure stability that Alfacip offers. Below you’ll find a curated collection of guides, comparisons, and safety tips that dive deeper into each of these topics, giving you practical takeaways you can apply today.