Fecal Transplant: How It Works, Who It Helps, and What to Expect
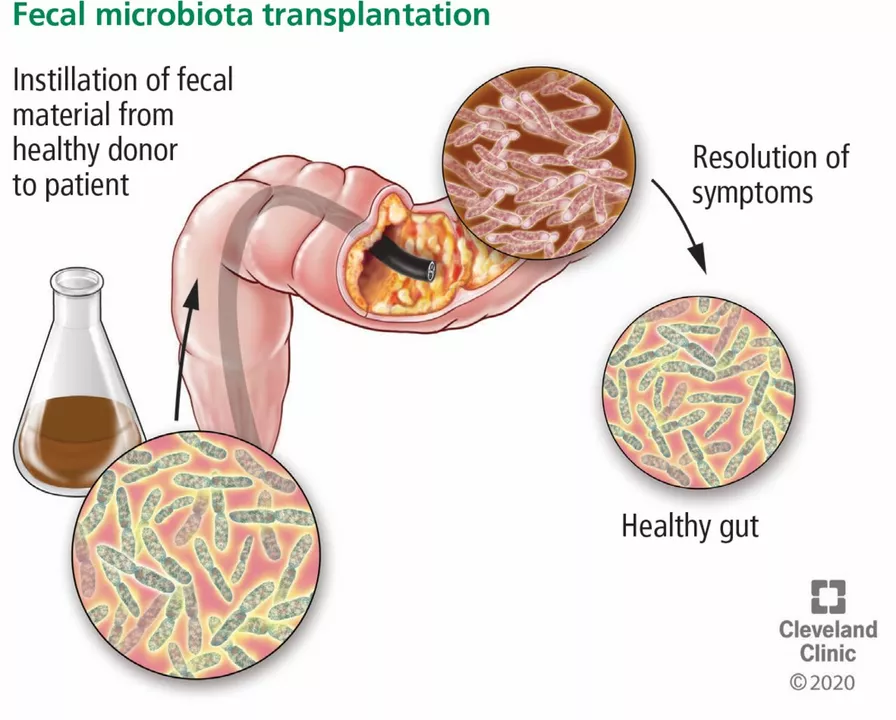
Ever heard of fecal transplant and wondered what it actually is? Put simply, it’s a way to restore healthy gut bacteria by transferring screened stool from a donor to a patient. That sounds odd, but for certain infections—especially recurring Clostridioides difficile (C. difficile)—it can be life-changing.
Who should consider it? Right now, the clearest use is for people with recurrent C. difficile infections that don’t respond to standard antibiotics. Doctors usually try one or more antibiotic courses first. If infections keep coming back, fecal microbiota transplantation (FMT) becomes a recommended option in many guidelines.
How the procedure works
There are three common ways to deliver donor material: colonoscopy, enema, or oral capsules. Colonoscopy puts the material directly into the colon, which is often effective but requires sedation. Enemas are less invasive but may not reach the entire colon. Pills are the easiest for patients—carefully processed, frozen stool is put into capsules you swallow over a short period.
Donor screening matters a lot. Clinics and stool banks test donors for infectious diseases, gut pathogens, and certain medical conditions. This reduces risk but can’t remove it completely. That’s why reputable centers follow strict protocols and document informed consent.
Benefits, risks, and what to expect after
Benefits: many people with recurrent C. difficile feel better quickly—diarrhea can stop within days, and long-term cure rates are high compared to repeated antibiotics.
Risks: most side effects are mild—bloating, gas, or temporary stomach upset. Rare but serious risks include transfer of infections or unexpected immune responses. Because of that, clinics track patients after the procedure and report outcomes.
Recovery is usually short. You might be advised to avoid certain medications or probiotics for a short time and follow a simple diet plan your clinic gives you. Always follow the clinic’s instructions about stopping or restarting antibiotics before the procedure.
How to find care: ask your gastroenterologist or infectious disease doctor if FMT is right for you. Some hospitals run FMT programs; there are also accredited stool banks that supply screened material to clinics. Check if your insurance covers it—coverage varies by location and reason for the transplant.
What about other uses? Researchers are testing FMT for conditions like ulcerative colitis, IBS, and metabolic disorders. Early results are mixed, and these uses are still experimental. If you’re curious, ask about clinical trials at major medical centers.
Questions to ask your provider: Am I a good candidate? How do you screen donors? Which delivery method do you recommend and why? What follow-up will I have? Clear answers help you weigh benefits and risks.
Bottom line: fecal transplant is a proven option for recurrent C. difficile and an active area of research for other gut problems. If you’re dealing with repeat infections, talk to your doctor about whether FMT could help you get back to normal life.