Hepatitis C Treatment: Fast Facts and Real Steps
Hepatitis C used to be a long, uncertain fight. Now most people are cured with 8–12 weeks of pills. These drugs — called direct-acting antivirals (DAAs) — attack the virus directly and work for more than 95% of patients. If you have HCV, getting treated now can stop liver damage and lower your risk of cancer.
Before you start
First, get the right tests: an HCV antibody test followed by an HCV RNA (PCR) to confirm active infection. Your doctor will check liver health with blood tests (ALT, AST), platelets, and often a fibrosis score like FIB‑4 or a FibroScan to see how much scarring you have. Also test for hepatitis B and HIV because co-infections change the plan.
Many modern regimens are pan-genotypic (they work across all HCV types), so genotype testing is less crucial than before — but your clinician will decide if it’s needed. Tell your provider about every medicine and supplement you take — some DAAs interact with statins, certain heart drugs, anticonvulsants, and herbal products like St. John’s wort.
What to expect during and after treatment
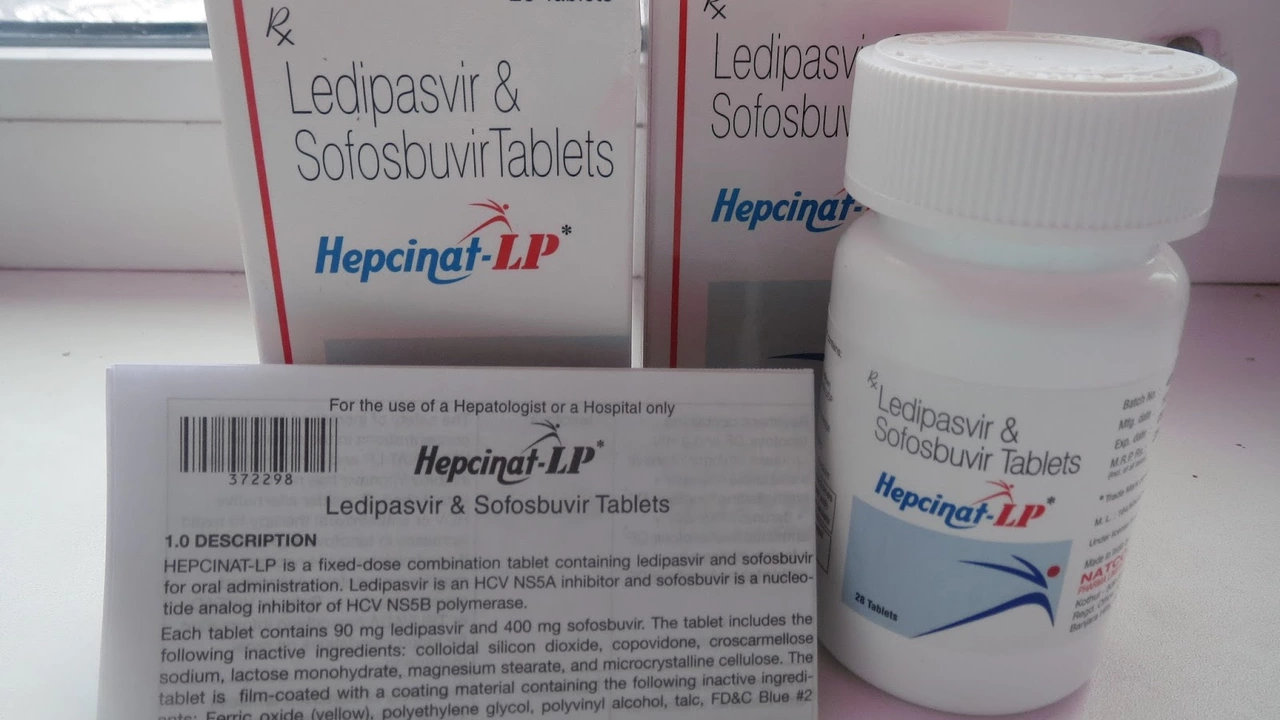
Common DAA combos you’ll hear about: sofosbuvir/velpatasvir (Epclusa), sofosbuvir/ledipasvir (Harvoni), and glecaprevir/pibrentasvir (Mavyret). Typical courses are 8, 12, or sometimes 24 weeks depending on prior treatment and cirrhosis. Side effects are usually mild — headache, tiredness, or nausea — and far fewer than older therapies.
About 12 weeks after finishing treatment your doctor will order an HCV RNA test. If it’s undetectable at week 12 (SVR12), you’re considered cured. Keep in mind: cure means the virus is cleared, but any existing liver scarring stays and needs follow-up. People with advanced fibrosis or cirrhosis should continue regular liver checks and cancer screening.
Special groups need tailored care. People with decompensated cirrhosis, pregnant people, or those with severe kidney disease should be managed by a specialist. People living with HIV usually can be treated safely, but therapy timing and interactions matter.
Cost and access vary. Generic versions and assistance programs can make treatment affordable in many countries. Telemedicine clinics often speed up testing and prescriptions. If you’re worried about cost, ask your clinic about patient assistance or generic options.
Final practical tips: get vaccinated for hepatitis A and B if you’re not immune, avoid alcohol while your liver heals, and don’t delay treatment — the pills work best before serious liver damage builds up. Talk to a provider you trust, bring a full meds list, and ask about drug interactions and follow-up testing. Treating hepatitis C now usually means a short, clear path to cure.