Pulmonary arterial hypertension (PAH): what you need to know
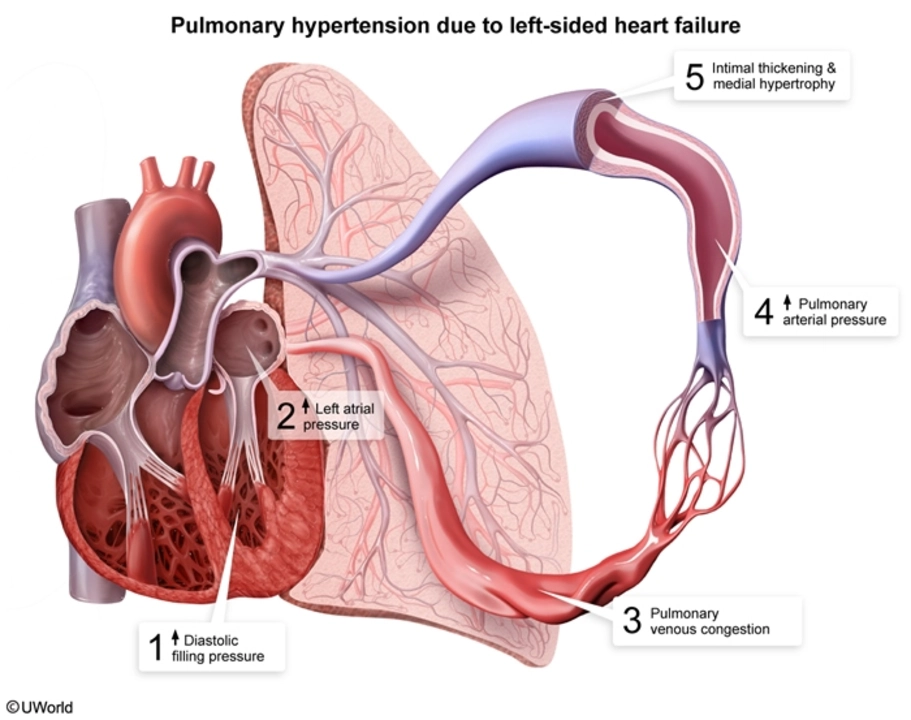
Pulmonary arterial hypertension (PAH) is high blood pressure in the arteries that carry blood from your heart to your lungs. It’s different from regular high blood pressure and can be serious if left untreated. If you’ve felt short of breath doing things that used to be easy, or you tire fast, PAH could be one of the causes worth checking.
How you spot PAH: symptoms and tests
Symptoms often start slowly: breathlessness with activity, feeling unusually tired, swelling in the ankles or belly, chest discomfort, or fainting spells. Those signs can look like other conditions, so doctors use tests, not just symptoms. Expect a few common tests: a basic exam and blood work, an ECG, a chest X-ray, and an echocardiogram (heart ultrasound). If those suggest PAH, you may be referred for a right heart catheterization — that’s the test that measures pressure in the lung arteries and confirms the diagnosis.
Other checks can include lung function tests, sleep studies, CT scans, and blood tests to rule out causes like autoimmune disease or liver problems. Keep a symptom diary (what you were doing when you felt short of breath, how long it lasted) — that helps your doctor track changes over time.
Treatment options and living with PAH
Treatment aims to lower pressure in the lung arteries, improve symptoms, and slow disease progression. There’s no one-size-fits-all plan. Common drug classes used for PAH include:
- Endothelin receptor antagonists (ERAs): examples are bosentan and ambrisentan.
- Phosphodiesterase-5 inhibitors (PDE5i): sildenafil and tadalafil are typical names.
- Prostacyclin analogs and receptor agonists: epoprostenol, treprostinil, and selexipag. These can be given by IV, pump, inhaled, or oral forms.
- Soluble guanylate cyclase stimulators: riociguat is one example.
Each medicine has pros and cons and possible side effects. That’s why PAH treatment is usually handled by specialists at a pulmonary hypertension center. Some people need combination therapy (two or more drugs) to control symptoms. Your doctor may also recommend oxygen, diuretics for swelling, blood thinners in select cases, and supervised exercise programs.
Practical tips: avoid heavy exertion that causes fainting, stay up-to-date on vaccines, check with your specialist before starting new meds or supplements, and talk to your doctor about pregnancy risks — PAH makes pregnancy high-risk for both mother and baby.
What to ask your doctor: What type of PAH do I have? Do I need more tests? What are treatment goals and side effects? Is a PH center nearby? When should I call for urgent help?
Finding care early and working with a PH team makes a real difference. If you suspect PAH, push for the right tests and a referral to a specialist. Small steps — tracking symptoms, asking focused questions, and following a tailored treatment plan — help you manage daily life better and protect your heart and lungs long term.