Stroke Prevention: Strategies, Tips, and Medication Insights
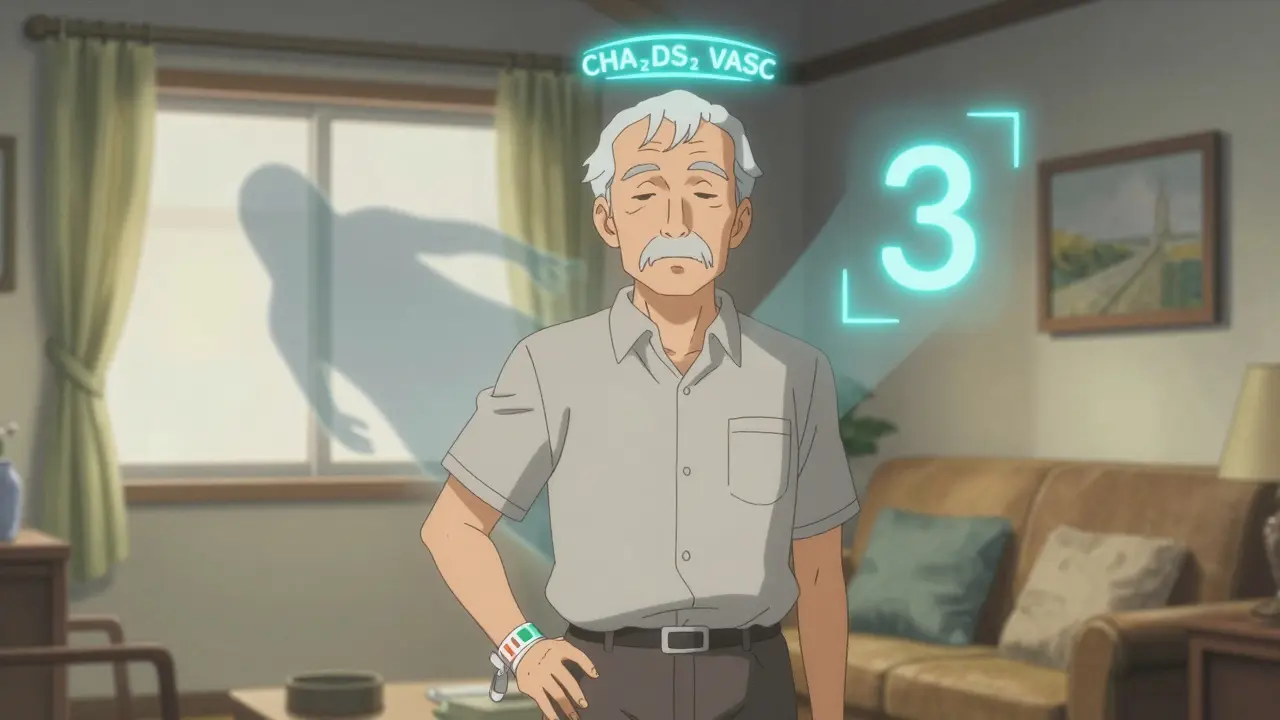
When talking about stroke prevention, the set of actions aimed at lowering the chance of a cerebrovascular accident. Also known as cerebrovascular risk reduction, it focuses on keeping the brain’s blood supply safe. Diabetes management, controlling blood sugar through medication, diet, and exercise is a core pillar, because high glucose levels damage blood vessels over time. Equally important is blood pressure control, maintaining systolic and diastolic numbers within a healthy range, since hypertension is the single biggest stroke risk factor. Finally, lifestyle modification, changing daily habits like diet, activity, and stress handling ties everything together. stroke prevention isn’t a one‑time checklist; it’s an ongoing process that blends medical and everyday choices.
High blood pressure, uncontrolled diabetes, and high cholesterol form the classic triad that drives most strokes. When these three clash, the vessels become stiff, narrowed, or clot‑prone, making a blockage or bleed more likely. Add smoking or excessive alcohol, and the damage accelerates. Stress isn’t just a feeling; chronic cortisol spikes raise blood pressure and impair glucose regulation, deepening the risk. Even seemingly harmless habits, like daily caffeine overuse, can nudge intra‑ocular pressure and influence overall vascular tone. Understanding these links helps you spot which habit to curb first.
Medication interactions are a hidden hazard in any prevention plan. For example, mixing metformin, a common diabetes drug, with alcohol can trigger lactic acidosis, a serious condition that stresses the cardiovascular system. Vitamin D analogues like alfacalcidol may support vessel health, but over‑supplementation can upset calcium balance, indirectly affecting blood pressure. Antihypertensives work best when you avoid foods that interfere with absorption, such as certain calcium‑rich meals. Knowing which drugs interact with everyday choices lets you keep the protective benefits without unintended side effects.
Changing everyday habits is where most people see quick wins. Swapping sugary drinks for water cuts both calorie intake and blood sugar spikes. Adding a 30‑minute brisk walk several times a week improves endothelial function, lowering blood pressure naturally. Stress‑relief techniques—deep breathing, meditation, or short breaks—reduce cortisol, which in turn eases hypertension. Limiting alcohol to one drink a day for women and two for men cuts both lactic acidosis risk and overall stroke chance. Small, consistent tweaks add up to a sturdier vascular system.
Regular health checks close the loop. Monitoring blood pressure at home gives you instant feedback on how lifestyle moves the needle. Annual eye exams can spot early signs of high intra‑ocular pressure, a marker for vascular strain. Kidney function tests, like checking for stone formation, reveal how well your body processes minerals that affect blood pressure. By tracking these metrics, you can adjust medication doses, address new risk factors, and stay ahead of potential problems before they turn into a stroke.
Below you’ll find a curated collection of articles that drill deeper into each of these areas. From detailed guides on how alcohol interacts with diabetes meds to side‑by‑side drug comparisons, the posts give you practical tools to fine‑tune your prevention plan. Whether you’re looking for diet tips, medication safety checks, or the latest research on risk factors, the resources here will help you build a stronger, stroke‑free future.