Understanding Diabetic Peripheral Neuropathy
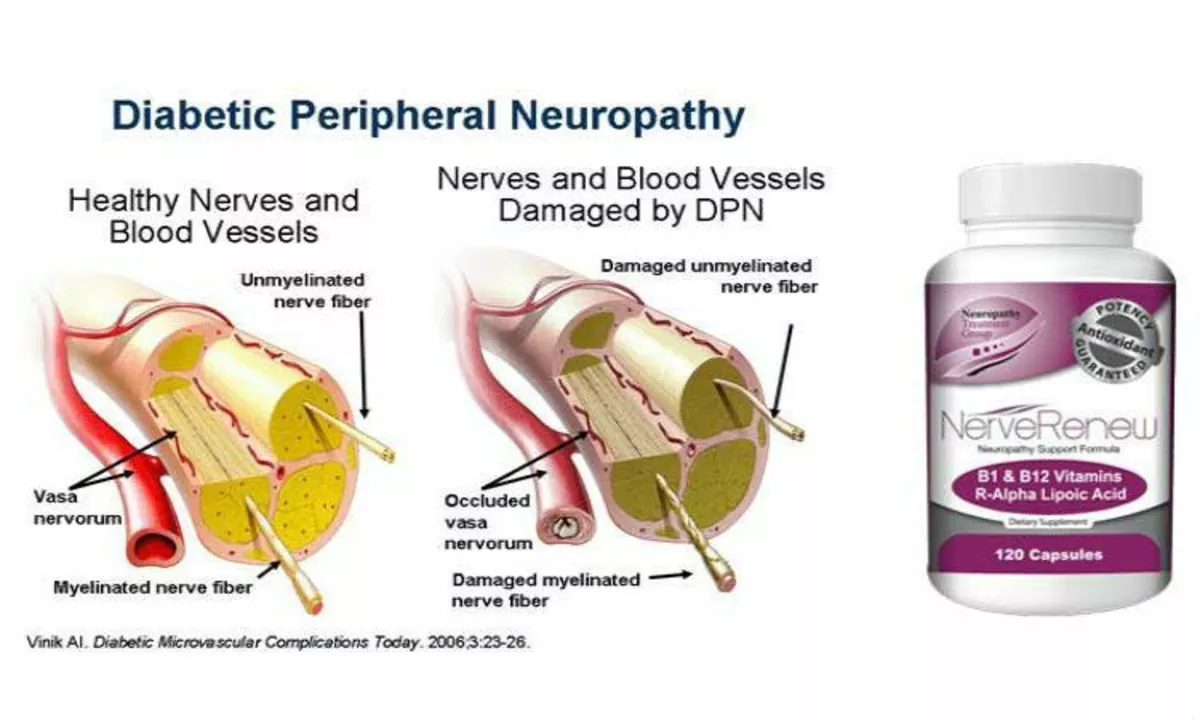
Before we dive into the link between diabetic peripheral neuropathy and cardiovascular disease, let's first get a clear understanding of what diabetic peripheral neuropathy is. Diabetic peripheral neuropathy is a type of nerve damage that occurs in people with diabetes. High blood sugar levels can damage nerve fibers throughout the body, but diabetic neuropathy most often affects nerves in the legs and feet.
There are different types of diabetic neuropathy, but the most common is peripheral neuropathy, which affects the nerves responsible for sensation, movement, and function in the arms and legs. Symptoms can include pain, tingling, numbness, and weakness in the extremities. These symptoms can range from mild to severe and can have a significant impact on a person's quality of life.
Cardiovascular Disease: An Overview
Cardiovascular disease is a broad term that covers a range of conditions affecting the heart and blood vessels. These conditions can include coronary artery disease, heart attack, stroke, heart failure, and many others. It is the leading cause of death worldwide, and people with diabetes are at a higher risk of developing cardiovascular disease than those without diabetes.
There are many factors that contribute to this increased risk, including high blood sugar levels, high blood pressure, obesity, and high cholesterol levels. However, another important factor that plays a role in the development of cardiovascular disease in people with diabetes is diabetic peripheral neuropathy.
How Diabetic Peripheral Neuropathy Affects the Heart and Blood Vessels
It is well-established that diabetic peripheral neuropathy can lead to an increased risk of cardiovascular disease. The connection between these two conditions is complex, and there are several ways in which diabetic neuropathy can negatively impact the heart and blood vessels.
First, diabetic neuropathy can cause damage to the nerves that control the heart and blood vessels, leading to a condition called autonomic neuropathy. This can affect the normal functioning of the heart, including its ability to pump blood efficiently and maintain a regular heartbeat. Autonomic neuropathy can also impair the blood vessels' ability to constrict and dilate properly, which can lead to poor blood flow and increased risk of blood clots.
The Role of Inflammation in Diabetic Neuropathy and Cardiovascular Disease
Another key factor linking diabetic peripheral neuropathy and cardiovascular disease is inflammation. Chronic inflammation is a common feature of both conditions and can contribute to the development of cardiovascular disease in people with diabetic neuropathy.
High blood sugar levels can trigger an inflammatory response in the body, leading to the production of inflammatory molecules and the activation of immune cells. This chronic inflammation can damage blood vessels and contribute to the formation of plaques in the arteries, which can eventually lead to a heart attack or stroke.
Reduced Sensation and Poor Wound Healing
Diabetic peripheral neuropathy can also contribute to poor wound healing and an increased risk of foot ulcers, which can have serious consequences for cardiovascular health. The reduced sensation that occurs with neuropathy can make it difficult for people with diabetes to notice cuts, sores, or other injuries on their feet.
Furthermore, poor blood flow resulting from damaged blood vessels can slow down the healing process, making it more likely for wounds to become infected and ulcerated. These foot ulcers can lead to serious complications, including amputation, and can significantly increase the risk of cardiovascular disease.
Managing Diabetic Peripheral Neuropathy to Reduce Cardiovascular Risk
Given the strong link between diabetic peripheral neuropathy and cardiovascular disease, it is crucial for people with diabetes to manage their neuropathy effectively in order to reduce their risk of developing serious heart and blood vessel problems. This includes maintaining good blood sugar control, which can help to prevent or slow the progression of neuropathy.
Other important steps include managing blood pressure and cholesterol levels, exercising regularly, maintaining a healthy weight, and quitting smoking. Additionally, regular foot care and check-ups are essential to detect and treat any foot problems early, before they become more serious.
Conclusion: The Importance of Early Intervention
In conclusion, diabetic peripheral neuropathy is a common and potentially serious complication of diabetes that can significantly increase the risk of cardiovascular disease. Understanding the connection between these two conditions and taking steps to manage neuropathy effectively can help to reduce this risk and improve overall health and well-being for people with diabetes.
Early intervention is key, so if you or a loved one has diabetes, it is important to work closely with your healthcare team to develop a comprehensive care plan that addresses both diabetic neuropathy and cardiovascular health.

Comments
Odin Zifer May 15, 2023 AT 01:58
They don't want you to know how the pharma giants push neuropathy meds just to keep you hooked on more prescriptions it’s a cash grab disguised as care
Paul Koumah May 22, 2023 AT 00:38
Look, managing blood sugar and staying active is the real game changer – no magic pill, just good habits
Erica Dello May 28, 2023 AT 23:18
First off, you *should* be using proper commas – "diabetic peripheral neuropathy" needs a comma after "diabetic" 😏 Also, the article missed a few hyphens – "high‑blood‑sugar" would be better
sara vargas martinez June 4, 2023 AT 21:58
When we examine the pathophysiology of diabetic peripheral neuropathy, it becomes evident that the microvascular changes are not isolated events but part of a systemic cascade that also predisposes patients to cardiovascular complications. The chronic hyperglycemic environment leads to the formation of advanced glycation end‑products, which in turn provoke oxidative stress and endothelial dysfunction. This endothelial dysfunction manifests as reduced nitric oxide bioavailability, impairing vasodilation and fostering a pro‑thrombotic state. Moreover, the autonomic fibers that regulate heart rate and vascular tone are particularly vulnerable to metabolic insults, resulting in altered heart rate variability and orthostatic hypotension. In parallel, the inflammatory milieu, characterized by elevated cytokines such as IL‑6 and TNF‑α, contributes to plaque instability within arterial walls. As the peripheral nerves lose their protective sensation, patients become less aware of minor injuries, leading to ulcer formation and subsequent infections that further exacerbate systemic inflammation. The resulting infection can precipitate sepsis, a known risk factor for myocardial infarction and stroke. Additionally, the chronic pain associated with neuropathy often leads to reduced physical activity, which compounds the risk by promoting sedentary behavior, weight gain, and dyslipidemia. Each of these factors-hyperglycemia, inflammation, autonomic dysfunction, and reduced mobility-creates a synergistic environment that accelerates atherosclerotic processes. Therefore, effective management must be multidimensional, targeting glycemic control, blood pressure, lipid levels, and lifestyle modifications simultaneously. Early screening for autonomic neuropathy using heart rate variability testing can identify patients at heightened cardiovascular risk before overt disease manifests. Foot care programs not only prevent ulceration but also serve as a window into the overall vascular health of the individual. In summary, the interplay between diabetic peripheral neuropathy and cardiovascular disease is mediated by a complex network of metabolic, inflammatory, and autonomic pathways, all of which demand comprehensive therapeutic strategies.
Todd Anderson June 11, 2023 AT 20:38
It is incumbent upon the discerning reader to appreciate that the nexus between neuropathic degeneration and cardiac pathology is not merely correlative but originates from a shared etiological substrate, namely chronic hyperglycemia, which inexorably compromises both neural and vascular integrity.
Dexter Smith June 18, 2023 AT 19:18
Indeed, the data underscore a mechanistic overlap; the autonomic fiber impairment directly influences myocardial perfusion, which corroborates the observed elevation in cardiovascular events among this cohort.
Cherish Capps June 25, 2023 AT 17:58
hey folks if you got any foot care tips feel free to share we all gotta look out for each other lol
Amy Carpenetti July 2, 2023 AT 16:38
I hear ya! gentle moisturizing and checking your toes daily can make a huge difference – stay safe
Crystal Newgen July 9, 2023 AT 15:18
Interesting read.
Hannah Dawson July 16, 2023 AT 13:58
While it may seem merely informative, the omission of socioeconomic disparities in access to care is a glaring oversight that perpetuates health inequities.
Julie Gray July 23, 2023 AT 12:38
One must consider that the mainstream medical narrative intentionally downplays the role of hidden corporate lobbying in shaping research priorities concerning neuropathy and heart disease.
Lisa Emilie Ness July 30, 2023 AT 11:18
Good info thanks