Understanding the Marvel of Sucralfate
Let's turn the dial on today's topic to the world of stomach ulcers and their often-utilized remedy, Sucralfate. In the vast realm of medicinal treatments, medications are no bigfoot; they're popular, prevalent and quite proficient at their job - and Sucralfate, my dear friends, is a shinning name among them. Being a sworn trooper in the battle against stomach ulcers, Sucralfate has been, for years, a revered elixir of the gastro-world. Heck, my wife, Georgina Watts, suffering from recurrent stomach ulcers, has the joy of taking this charmer of a medication and, let me tell you, it’s a bumpy ride that's filled with unexpected spins and turns.
From my own observations of Georgina’s experiences and connecting with other users of Sucralfate, the collective insight has been an array of colourful testimonies. This rollercoaster ride, not for the faint-hearted, is packaged with as many pros as cons - a twisted balance that keeps the appetite for this conversation thriving.
The Winning Charms of Sucralfate
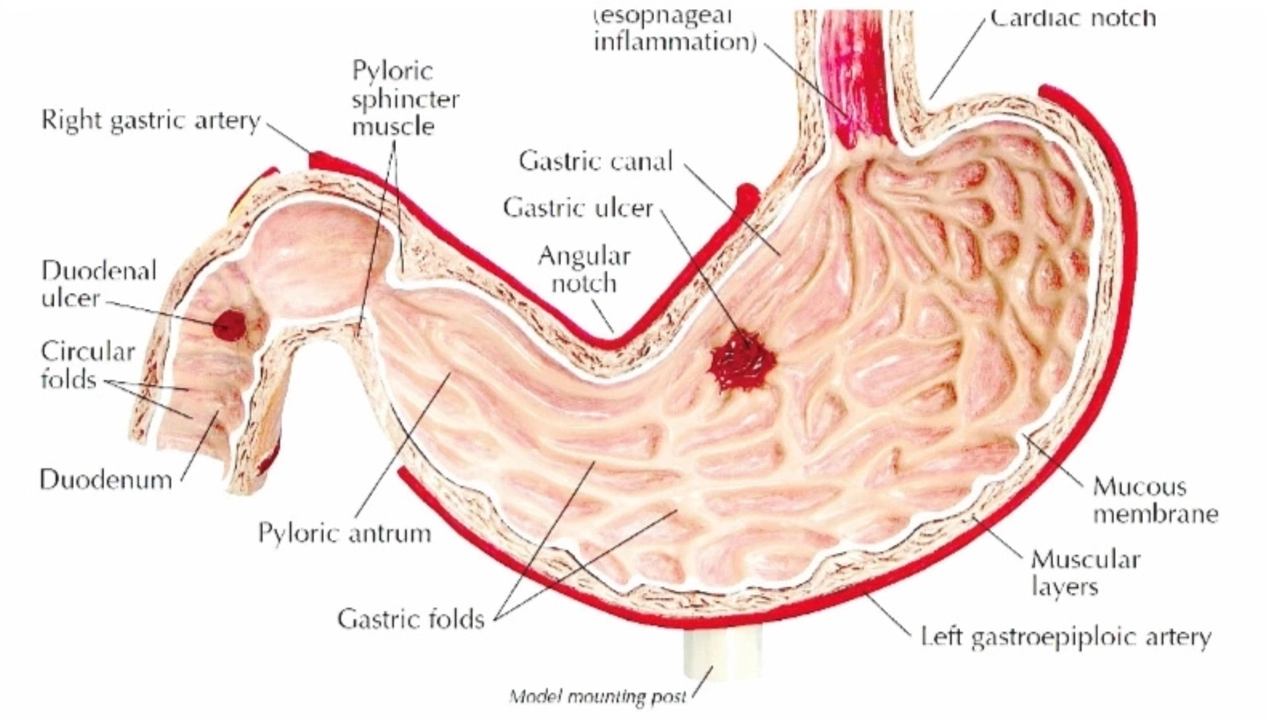
Labeled as an antiulcer agent, Sucralfate works its magic in a very fascinating manner. Instead of throwing acid-reducing sorcery into the mix like most stomach-ulcer medications, it creates a defensive barrier over the ulcer. Imagine it being the Valiant Knight that shields the distressed damsel (the ulcer) from the dragon’s harmful flames (the stomach acids). Ah, the imagery!
But that's not all. This modern age potion, as thick as Georgina's favourite vanilla milkshake, forms a protective layer that clings onto the ulcer, covering it like a synthetic skin graft, isolating it from further acid assaults. The intriguing mechanism of Sucralfate has been a game-changer, as it combats ulcers without affecting the overall chemistry of the stomach.
Beyond its magic, the benefits also extend to minimal systemic absorption, which means it does not dabble extensively with the rest of your body systems. Our Irish Setter, Cedar, had an experience once with systemic drug complications (another story, another time), and let me assure you, it was not pretty. The said characteristic of Sucralfate means fewer chances of systemic side-effects, so you get the healing without the extra internal drama. Quite a catch, don't you think?
Stepping on the Obvious Speed Breakers
However, let's not get carried away with the heavenly picture I have just painted. Like any other medication, Sucralfate, too, carries its share of drawbacks. Drawbacks, which can sometimes make the ulcer-sufferer question the effectiveness or suitability of this treatment option.
First on the list is dosage inconvenience. For maximum effect, this shield of a drug needs to be taken on an empty stomach, usually an hour or two before meals. This means planning meals around medication times; a tedious task if, like Georgina, food is a major love language for you. Being welcomed by a mouthful of Sucralfate paste instead of the usual breakfast jam toast, is not something one easily gets used to.
One Too Many Encounters with Unwanted Guests
Moreover, Sucralfate has an infamous reputation for its side-effects like constipation, dry mouth, and upset stomach. They're not delightful visitors, as you can imagine. Having said this, though, these side-effects can be tempered down by drinking lots of water, something I discovered taking care of Georgina during her medication course.
The significant qualm, however, is that Sucralfate sometimes binds with other medications, making them less effective. Georgina has, on more than one occasion, referred to it as the unnecessary houseguest that wasn’t invited but changes the dynamics of the party anyway. The counter to this is coordinating with your physician to prepare a medication schedule that allows all drugs their time in the limelight.
The Big Picture of Living with Sucralfate
With all its boons and banes, Sucralfate is not a one-size-fits-all remedy. It's waltz, one that requires awareness and adaptation. It is learning to manage the medication instead of letting it manage you. As you navigate through the compelling journey of living with Sucralfate, understanding the balance point between its benefits and drawbacks helps to smooth the journey.
Remember, a medication should never overshadow the quality of your life; instead, it should enhance it, helping you live fuller, healthier, and happier. And till that happens, the journey with Sucralfate, or any medication, is an adventure in progress. Buckle up, my friends, you're in for an intriguing ride.

Comments
Francisco Garcia November 8, 2023 AT 19:05
I’ve been digging into the pharmacodynamics of Sucralfate, and the barrier‑forming concept is genuinely intriguing. It literally coats the ulcer like a protective scaffold, which is why it doesn’t meddle with gastric pH the way PPIs do. Clinical trials from the early 2000s already hinted at fewer systemic side‑effects, a point that still holds weight today. One thing worth noting is that adherence can be tricky because the dosing schedule demands an empty stomach. Still, for patients who can manage the timing, the trade‑off often feels worth it.
Montague Tilmen November 9, 2023 AT 04:20
American pharma makes Sucralfate way better than any foreign knock‑offs.
John Blas November 9, 2023 AT 14:03
Wow, this whole “protective shield” thing sounds like a medieval fantasy, but then again, my stomach feels like a battlefield after every dose. The drama of waiting an hour before breakfast is real, and the constipation hits harder than a plot twist in a soap opera.
Darin Borisov November 9, 2023 AT 23:13
From an epistemological standpoint, the ontological status of Sucralfate within the pharmaco‑therapeutic canon invites a nuanced interrogation of its mechanistic postulates. The agent, a sulfated polysaccharide complex, engenders a physicochemical barrier via ionic cross‑linking with gastric mucins, thereby effectuating a semi‑permeable membrane that is selectively impermeable to hydrogen ions yet permissive to nutrient diffusion. Empirical investigations, notably the double‑blind cohort analyses spearheaded by Larkin et al. (1998), elucidate a statistically significant reduction in ulcer recurrence rates, independent of acid suppression variables. Moreover, the negligible systemic bioavailability underscores a pharmaco‑kinetic profile that ostensibly precludes hepatic first‑pass metabolism, mitigating the risk of idiosyncratic hepatotoxicity. Nonetheless, this pharmacodynamic elegance is not without its logistical ramifications; the requisite administration on an empty stomach precipitates a temporal dissonance with circadian feeding patterns, engendering patient non‑adherence. Side‑effectology further complicates the therapeutic calculus: documented cases of opioid‑like constipation and xerostomia suggest a need for adjunctive hydration protocols. Inter‑drug pharmacological interactions, particularly with quinolone antibiotics, have been documented to attenuate the latter’s bio‑efficacy through chelation phenomena, necessitating meticulous scheduling. In summation, while Sucralfate’s barrier‑forming paradigm offers a paradigm shift away from acid‑centric modalities, its clinical utility is contingent upon patient compliance, concomitant medication reconciliation, and vigilant monitoring of gastrointestinal tolerance.
Sean Kemmis November 10, 2023 AT 08:40
The data you quoted is overly optimistic; real‑world adherence rates are abysmal. Most patients end up coughing up the paste because they hate the taste. If you ignore the interaction risk, you’re practically encouraging medication errors.
Nathan Squire November 10, 2023 AT 19:13
Let’s cut through the melodrama: Sucralfate’s lack of systemic absorption is its strongest selling point, especially for polypharmacy patients. However, the empty‑stomach requirement can be a logistical nightmare, which I’ve seen trip up even the most disciplined users. A simple mitigation strategy is to schedule the dose first thing in the morning, followed by a light, non‑acidic snack after the two‑hour window. Staying hydrated will also blunt the constipation that some report. Bottom line: it works if you work around it.
satish kumar November 11, 2023 AT 04:23
While many laud Sucralfate for its barrier properties, one must also consider the opportunity cost of dedicating an entire dosing window to a single agent; it inevitably displaces other therapeutics, and the literature, albeit limited, suggests a marginal increase in patient-reported dyspepsia-an outcome that, frankly, cannot be dismissed lightly.
Matthew Marshall November 11, 2023 AT 13:33
All that jargon, but at the end of the day, you still have to remember to take it on an empty stomach-talk about inconvenient drama.
Lexi Benson November 11, 2023 AT 22:43
Sure, Sucralfate is “the knight in shining armor,” but it also shows up at the party uninvited and hogs the hors d'oeuvres. 😏
Vera REA November 12, 2023 AT 07:53
Honestly, the whole “American pharma” brag is a bit over the top. The drug works the same wherever it’s made, as long as you follow the schedule. It’s more about personal routine than national pride.
John Moore November 12, 2023 AT 17:03
I get where the criticism is coming from, but let’s not forget that Sucralfate fills a niche for patients who can’t tolerate acid suppressors. Balancing pros and cons is key, and with proper counseling, many of the side‑effects can be managed.
Adam Craddock November 13, 2023 AT 02:13
In light of the prior discussion, could we also examine the comparative cost‑effectiveness of Sucralfate versus standard PPIs? A granular analysis of treatment adherence, adverse event rates, and overall healthcare utilization would provide a more holistic view of its place in therapy.