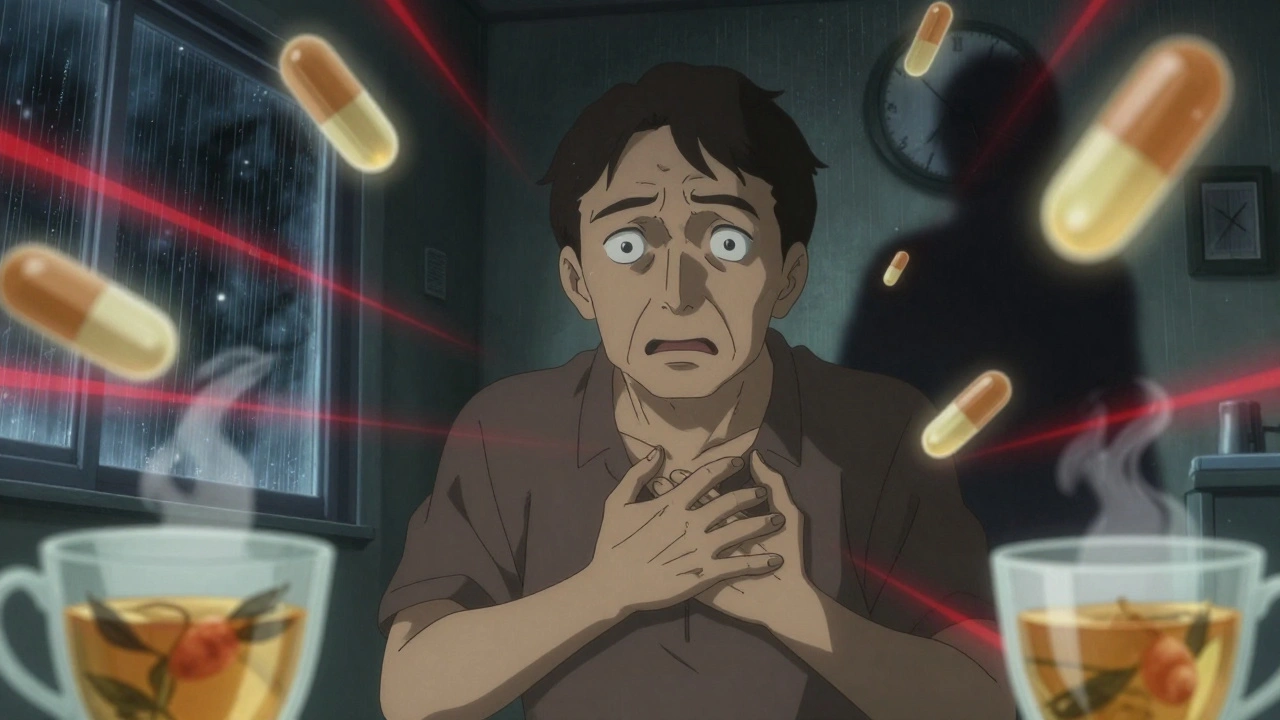
It’s easy to think that taking a few pills together is harmless. You’ve got your blood pressure med, your painkiller, your multivitamin, and maybe that herbal tea your cousin swears by. But what if one of those is quietly messing with another? Drug interactions don’t always scream for attention. Sometimes they whisper-fatigue, a weird rash, dizziness-and you brush it off as stress, aging, or just "feeling off." But in some cases, that whisper can turn into a life-threatening shout. Knowing when to seek medical help for a suspected drug interaction isn’t just smart-it can save your life.
What Counts as a Dangerous Drug Interaction?
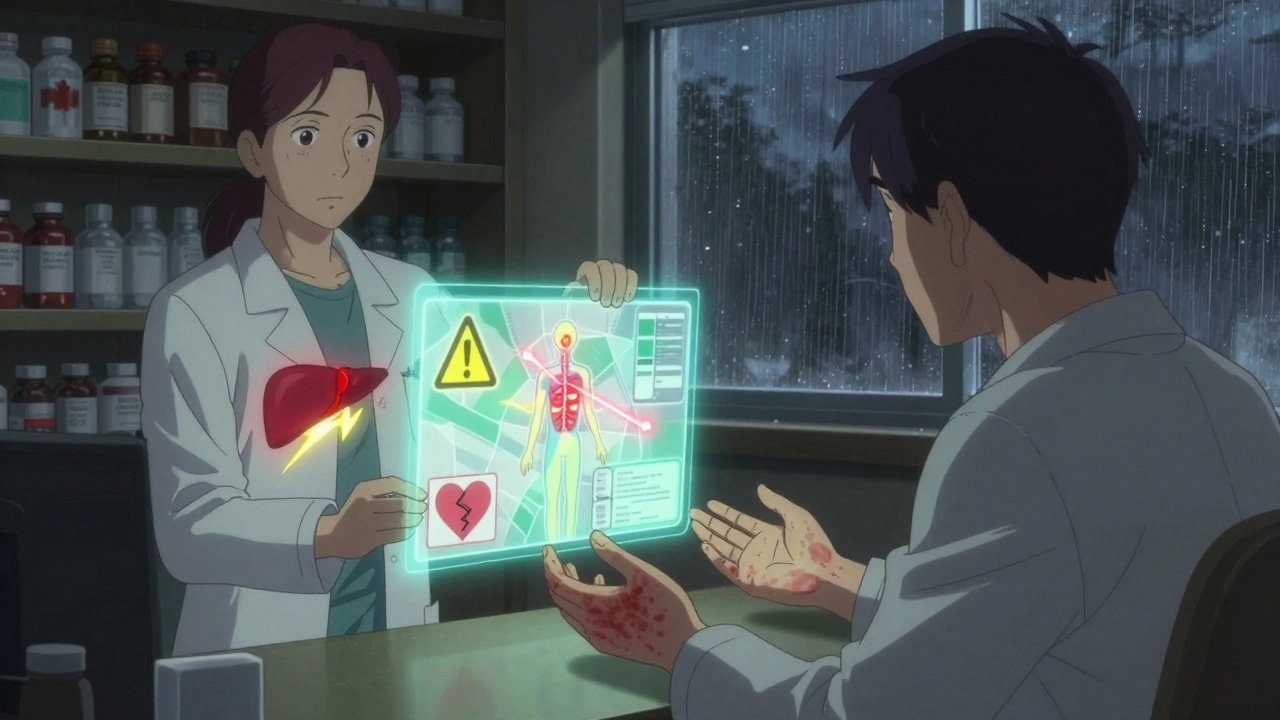
A drug interaction happens when one substance changes how another works in your body. This could be another prescription, an over-the-counter pill, a supplement, even food or alcohol. The FDA says these interactions can make a drug less effective, cause new side effects, or make its effects too strong. The most dangerous ones happen with drugs that have a narrow therapeutic index-meaning the difference between a helpful dose and a harmful one is tiny. Warfarin, digoxin, and phenytoin fall into this category. A 20% shift in blood levels can lead to a stroke, heart failure, or seizures. About 60% of serious interactions are drug-drug. Another 20% come from food or drink-like grapefruit juice killing the effect of statins. The rest involve your existing health conditions. For example, taking decongestants with high blood pressure can spike your numbers dangerously. The CDC reports that drug interactions send 1.3 million people to U.S. emergency rooms every year. Around 350,000 of them end up hospitalized. And here’s the kicker: 40% of those hospitalizations could’ve been avoided.Symptoms That Demand Immediate Emergency Care
If you’re taking multiple medications and suddenly feel like something’s very wrong, don’t wait. Some reactions escalate in minutes. Call 911 or go to the nearest ER if you have any of these:- Difficulty breathing or oxygen levels below 90% (measured by a pulse oximeter)
- Swelling of your face, lips, tongue, or throat-this can block your airway in under 20 minutes
- Systolic blood pressure dropping below 90 mmHg with a heart rate over 120 bpm
- A seizure lasting more than 2 minutes
- Loss of consciousness or confusion where you can’t answer simple questions
- Body temperature above 41.1°C (106°F), rigid muscles, and extreme agitation-signs of serotonin syndrome
- High fever over 40°C (104°F), dark urine, and muscle pain-possible neuroleptic malignant syndrome
Symptoms That Need a Doctor Within 24 Hours
Not every interaction crashes your system right away. Some build slowly. If you notice any of these, call your doctor or pharmacist today-not tomorrow, not next week:- A widespread rash covering more than 30% of your skin, especially if it’s blistering or peeling-could be DRESS syndrome
- Fever above 38.5°C (101.3°F) that lasts more than 48 hours, especially if you’re on antibiotics or seizure meds
- Unexplained bruising, nosebleeds, or tiny red dots on your skin-signs of low platelets
- Yellowing of your skin or eyes, dark urine, or right-side abdominal pain-possible liver damage
- Urinating much less than usual, swelling in your legs, or a sudden rise in creatinine levels-could mean kidney injury
When Two Symptoms Together Mean Trouble
The American College of Emergency Physicians has a simple rule: if you have two or more of these symptoms at the same time, get help fast:- Heart rate over 100 bpm
- Breathing faster than 20 times per minute
- Excessive sweating
- Dilated pupils
- Twitching muscles or overactive reflexes
- Shaking or tremors
Why People Wait Too Long (And Why That’s Dangerous)
A 2022 survey by the National Community Pharmacists Association found that 58% of people waited more than 12 hours before seeking help for suspected drug interactions. Why? Because they thought it was "just a side effect" or "not that bad." On MedHelp, 72% of users who later needed emergency care said they dismissed early symptoms as normal fatigue or indigestion. Dr. Michael Wolf’s 2022 JAMA study found that 68% of patients couldn’t identify serious interaction symptoms from the tiny print on their medication leaflets. The language is confusing. "May cause dizziness" doesn’t tell you when dizziness becomes dangerous. That’s why you need to know the red flags-not just read the pamphlet.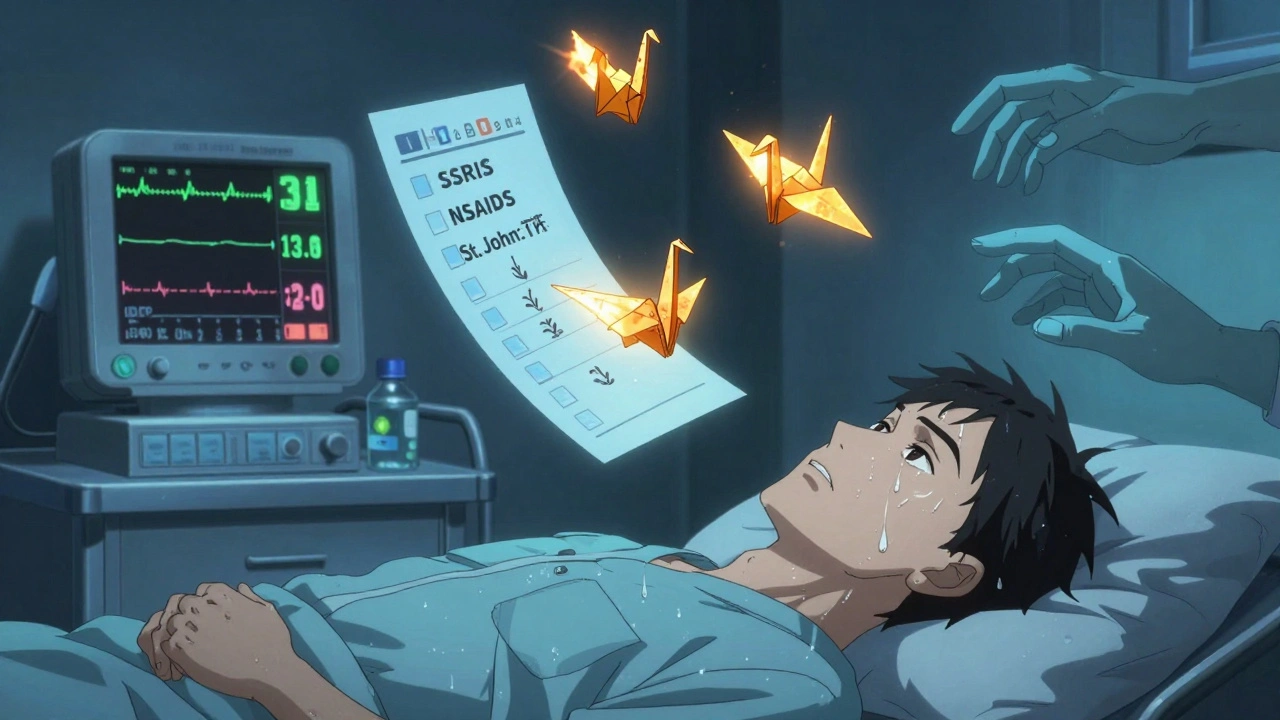
What You Can Do Right Now
If you take five or more medications-which 45% of adults over 65 do-you’re at high risk. The Journal of the American Geriatrics Society says the chance of a major interaction jumps to 57% with that many drugs. Here’s what to do:- Keep a current list of everything you take: prescriptions, OTC meds, vitamins, herbs, even CBD or melatonin
- Use a reliable drug interaction checker like Drugs.com or Lexicomp (updated daily) and input ALL substances
- Ask your pharmacist to review your list every time you pick up a new prescription
- Follow the STOP protocol: Stop the suspected med, Telephone your provider, Observe symptoms, Present all containers at your appointment

Comments
Ariel Nichole December 11, 2025 AT 17:02
Really glad someone laid this out so clearly. I used to think my dizziness was just stress until I started tracking my meds and realized my blood pressure pill was clashing with that turmeric supplement I was taking. Talk about a wake-up call.
Now I keep a little notebook in my wallet with everything I take. Even the gummy vitamins. My pharmacist laughs but says it’s the smartest thing she’s seen all week.
john damon December 12, 2025 AT 04:28
bro i took otc cold med + my antidepressant and thought i was just "feeling weird" 😅 turned out i was one step away from serotonin syndrome. hospital trip. no joke. just don’t mess around.
matthew dendle December 12, 2025 AT 19:20
so let me get this straight... you want people to read a 2000 word essay just to not die from mixing tylenol and wine? 🤦♂️ why dont they just put BIG RED LETTERS ON THE BOTTLE instead of hiding it in tiny print next to "may cause drowsiness"
Lisa Stringfellow December 13, 2025 AT 07:14
Of course this is such a well-researched article. Everyone knows how to read a label. The real problem is people who take 12 different pills and then blame the doctor when they feel bad. It’s not the meds-it’s the chaos.
Kristi Pope December 13, 2025 AT 10:47
Love this. Seriously. I used to roll my eyes at my grandma’s little pill organizer but now I get it. It’s not just about remembering to take them-it’s about seeing the whole picture.
My mom’s on 7 meds and we do a monthly check-in. She says it’s like a mini therapy session. Turns out talking about your pills helps you feel less alone with them.
Jimmy Kärnfeldt December 15, 2025 AT 02:09
It’s wild how we treat our bodies like machines that don’t talk back. We’ll ignore the hum, the flicker, the weird noise… until it breaks.
But your body’s always whispering. The trick is learning to listen before it screams. This post is basically a crash course in reading your own signals.
And yeah, poison control is a secret superhero. They don’t judge. They just help. Call them. Even if you’re not sure. It’s what they’re for.
Katherine Liu-Bevan December 16, 2025 AT 22:38
Important clarification: DRESS syndrome typically presents with fever, rash, lymphadenopathy, and internal organ involvement. The rash is often morbilliform or maculopapular and evolves over days. Early recognition is critical, as mortality can reach 10% if untreated.
Also, ALT >120 U/L is a red flag, but AST/ALT ratio and bilirubin levels should be evaluated together. Always correlate labs with clinical presentation.
Courtney Blake December 16, 2025 AT 22:49
USA has the best healthcare system in the world... until you need to know how not to kill yourself with your own meds. Why is this even a problem? Why do we need Reddit to teach people basic safety? We’re falling apart.
Aman deep December 17, 2025 AT 02:36
Man this hit home. I’m from India and we just grab meds from the pharmacy without even asking. My uncle took antibiotics with his blood thinner and ended up in ICU. No one knew it was dangerous.
Now I tell everyone: write down everything. Even the turmeric paste your aunt makes. That stuff can thin your blood too. 😅
Eddie Bennett December 18, 2025 AT 10:37
Been there. Took melatonin + trazodone for sleep and woke up feeling like my brain was vibrating. Thought I was having a panic attack. Turned out it was a mild serotonin thing. Called my doc, they said "cool, you’re lucky you didn’t wait."
Now I check everything on Drugs.com. Even my gummy worms. No joke.
Sylvia Frenzel December 19, 2025 AT 19:13
Another article telling us what we already know. Meanwhile, my insurance won’t cover the pharmacist consult, the interaction checker app costs $15/month, and my doctor’s office takes 3 weeks to return a call.
So thanks for the awareness... now fix the system.
Paul Dixon December 20, 2025 AT 09:49
My grandma’s pharmacist sits with her for 20 minutes every time she picks up a new script. She calls it "meds bingo"-crossing out the ones that don’t play nice.
Best part? The pharmacist remembers her allergies, her tea, her CBD oil, even the fish oil she swears by. That’s the kind of care we need more of.
Vivian Amadi December 20, 2025 AT 14:49
If you’re taking more than 5 meds, you’re not managing your health-you’re playing Russian roulette with your organs. Stop being lazy. Get your meds reviewed. Period.
Monica Evan December 21, 2025 AT 13:15
Just got back from my mom’s 78th birthday. She’s on 9 meds, 3 supplements, and a daily herbal tea blend she calls "the elixir".
She didn’t know the tea had kava-same class as her anxiety med. We found out because she started shaking and couldn’t walk straight. Called poison control. They said "call your doctor now, not tomorrow."
Now we do monthly med check-ins. It’s awkward. But she’s alive. And that’s what matters.
Taylor Dressler December 22, 2025 AT 05:05
One thing I wish more people knew: even "natural" doesn’t mean safe. St. John’s Wort interacts with over 50 drugs. Garlic supplements thin blood. Ginger can mess with diabetes meds.
Just because it comes from a plant doesn’t mean your body won’t treat it like a chemical bomb.
Always check. Always ask. Always write it down.