Antiplatelet Therapy: What It Is, How It Works, and What You Need to Know
When your blood starts to clot too easily, it can block arteries and trigger a heart attack or stroke. That’s where antiplatelet therapy, a treatment that stops blood platelets from clumping together to prevent dangerous clots. Also known as platelet inhibition, it’s one of the most common long-term treatments for people with heart disease, after stents, or following a stroke. Unlike blood thinners like warfarin that slow down the whole clotting process, antiplatelet drugs target just one part: the platelets. These are tiny cell fragments in your blood that rush to injury sites and stick together. In a healthy person, that’s good. In someone with clogged arteries, it’s life-threatening.
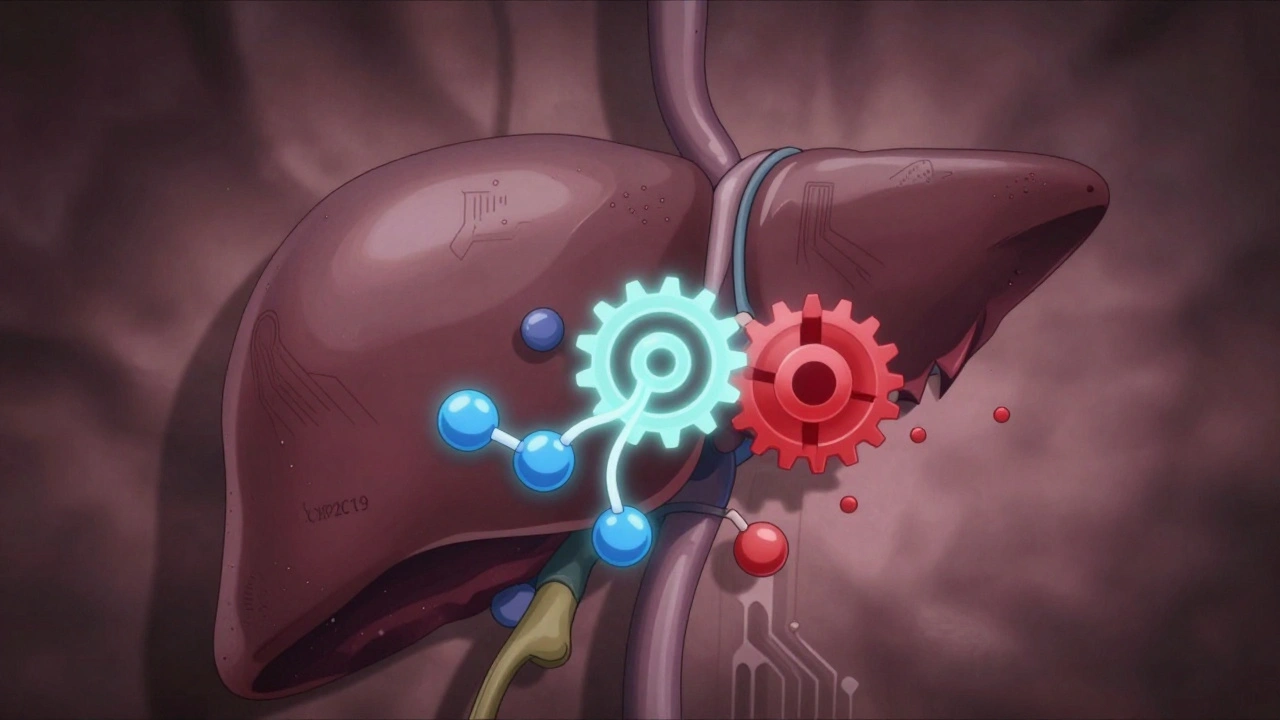
Most people on antiplatelet therapy take aspirin, a low-dose daily pill that has been used for decades to reduce clotting risk. Also known as acetylsalicylic acid, it’s cheap, widely available, and works for millions. But many also take clopidogrel, a stronger drug often paired with aspirin after a heart attack or stent placement. Also known as Plavix, it blocks a different pathway in platelets to keep them from activating. Other options include ticagrelor and prasugrel—drugs used when aspirin alone isn’t enough or when someone can’t tolerate it. These aren’t one-size-fits-all. Your doctor picks based on your history, risk level, and how your body responds.
Antiplatelet therapy isn’t without risks. Bleeding is the big one. A cut that won’t stop, nosebleeds, or even internal bleeding can happen. That’s why you never stop these meds without talking to your doctor—even if you’re scheduled for surgery. Some people also develop stomach upset or ulcers, especially with long-term aspirin use. And while these drugs prevent clots, they don’t fix the underlying problem. You still need to manage cholesterol, blood pressure, and lifestyle factors.
The posts below cover real-world issues you might face with these drugs: how to handle missed doses, what to do if you bleed, why some generics work differently than others, and how insurance fights to limit your access. You’ll also find info on drug interactions—like how mixing antiplatelets with certain supplements or painkillers can raise your bleeding risk. Whether you’re on one of these meds now or just starting, this collection gives you the practical knowledge to stay safe and get the most out of your treatment.