CYP2C19: What It Is, How It Affects Your Medications, and Why It Matters
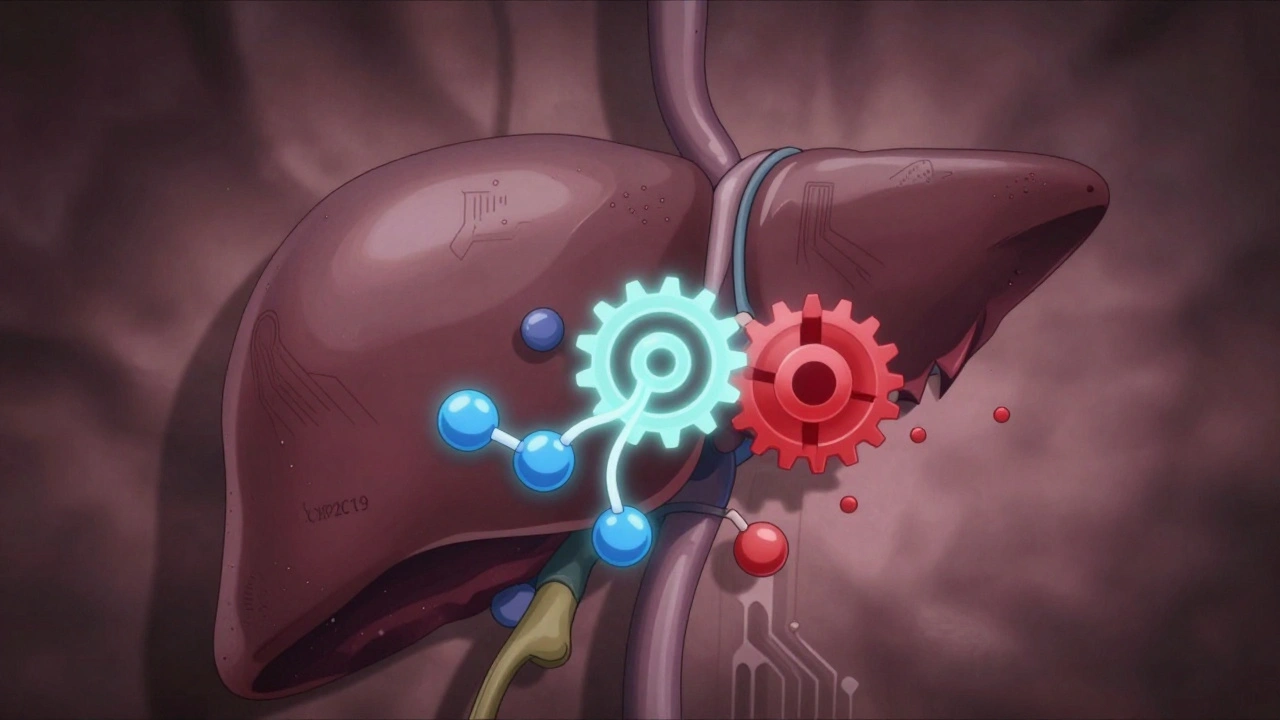
When your body breaks down medications, it doesn’t just guess—it follows a precise biological script. One of the main authors of that script is CYP2C19, a liver enzyme that metabolizes nearly 10% of commonly prescribed drugs. Also known as cytochrome P450 2C19, this enzyme is the reason why two people taking the same pill at the same dose can have wildly different results. Some people process drugs too fast, others too slow—and it’s not about their weight, age, or diet. It’s often written in their DNA.
CYP2C19 doesn’t work alone. It’s part of a family of enzymes called cytochrome P450, and it’s especially busy with drugs like clopidogrel (Plavix), proton pump inhibitors like omeprazole, antidepressants like citalopram, and anti-seizure meds like phenytoin. If your CYP2C19 is a slow metabolizer, clopidogrel might not work at all, raising your risk of a heart attack. If you’re a fast metabolizer, you might need a higher dose of omeprazole just to control acid reflux. This isn’t rare—it’s common. Up to 30% of people of Asian descent carry a gene variant that makes CYP2C19 less active. In Europeans, about 2-5% are ultra-rapid metabolizers, meaning drugs vanish from their system before they can help.
This isn’t science fiction. It’s clinical reality. Hospitals and clinics are starting to test for CYP2C19 variants before prescribing certain drugs. The FDA even includes pharmacogenomic information on labels for drugs like clopidogrel and voriconazole. But most doctors still don’t order these tests. Why? Cost, access, and lack of awareness. Still, if you’ve ever been told a medication "didn’t work" or caused unexpected side effects, your CYP2C19 status might be the missing piece.
Understanding CYP2C19 isn’t about complex genetics. It’s about getting the right dose, the right drug, the first time. It’s why some people need five different antidepressants before finding one that helps, while others respond to the first try. It’s why your uncle’s blood thinner didn’t prevent his stroke, and why your friend’s stomach medication suddenly stopped working. This enzyme affects who gets relief, who gets sick, and who ends up in the ER because a "safe" drug turned dangerous.
Below, you’ll find real-world posts that dig into how CYP2C19 connects to drug interactions, generic substitutions, adverse events, and why your prescription might not be working—even if it’s "supposed to." You’ll learn how to ask the right questions, spot hidden risks, and understand why two people on the same meds can have opposite outcomes. This isn’t theory. It’s what’s happening in pharmacies and clinics right now—and it’s something you can act on today.