Osteoporosis Medications: What Works, What to Avoid, and How to Stay Strong
When your bones start to thin, it’s not just about getting older—it’s about osteoporosis medications, drugs designed to slow bone loss and lower fracture risk in people with low bone density. Also known as bone-strengthening drugs, these medications are often the difference between staying active and facing a broken hip or spine. Osteoporosis doesn’t always cause symptoms until something breaks, which is why knowing what treatments exist—and which ones actually help—is critical.
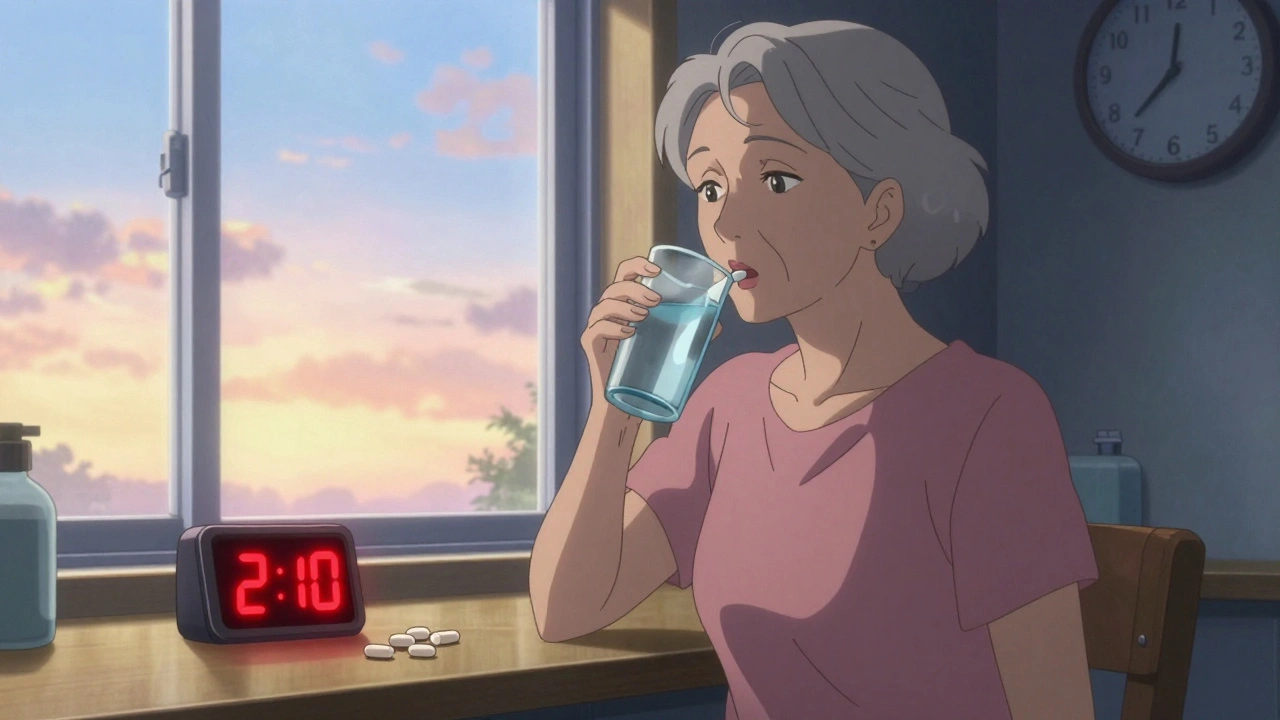
Bisphosphonates, a class of drugs that stop bone breakdown by targeting cells that dissolve bone tissue. Also known as bone resorption inhibitors, they include common prescriptions like alendronate (Fosamax) and risedronate (Actonel). These are usually the first line of defense because they’re effective, affordable, and have decades of real-world use behind them. But they’re not the only option. Denosumab, a monthly injection that blocks a protein responsible for bone loss. Also known as RANK ligand inhibitor, it works differently than bisphosphonates and is often used when pills don’t work or cause stomach issues. Then there’s teriparatide, a daily injection that actually builds new bone—rare among osteoporosis drugs. It’s powerful but expensive and limited to two years of use.
But meds alone won’t fix weak bones. Calcium, the main mineral your bones are made of. Also known as bone mineral, it’s not just a supplement—it’s the foundation. You need about 1,200 mg a day, mostly from food, but many people fall short. And without enough vitamin D, the hormone your body uses to absorb calcium from food. Also known as calciferol, it’s essential for any osteoporosis treatment to work. If your vitamin D is low, even the strongest drug won’t help. Most doctors check both levels before prescribing anything.
Some meds come with risks. Long-term bisphosphonates can rarely cause jaw bone problems or unusual thigh fractures. Denosumab requires strict timing—if you miss a dose, bone loss can speed up fast. And while calcium supplements are common, too much can raise heart risks. That’s why treatment isn’t one-size-fits-all. Your age, fracture history, kidney function, and even how well you swallow pills all matter.
The posts below don’t just list drugs—they show you what actually happens when people take them, how side effects show up in real life, and what to watch for when switching treatments. You’ll find comparisons between common options, warnings about interactions with other meds, and insights into why some people see results while others don’t. Whether you’re just starting treatment or trying to figure out why your current plan isn’t working, the real stories here will help you ask the right questions and make smarter choices.