Stomach Ulcers: Spot Them Fast and Know What Helps
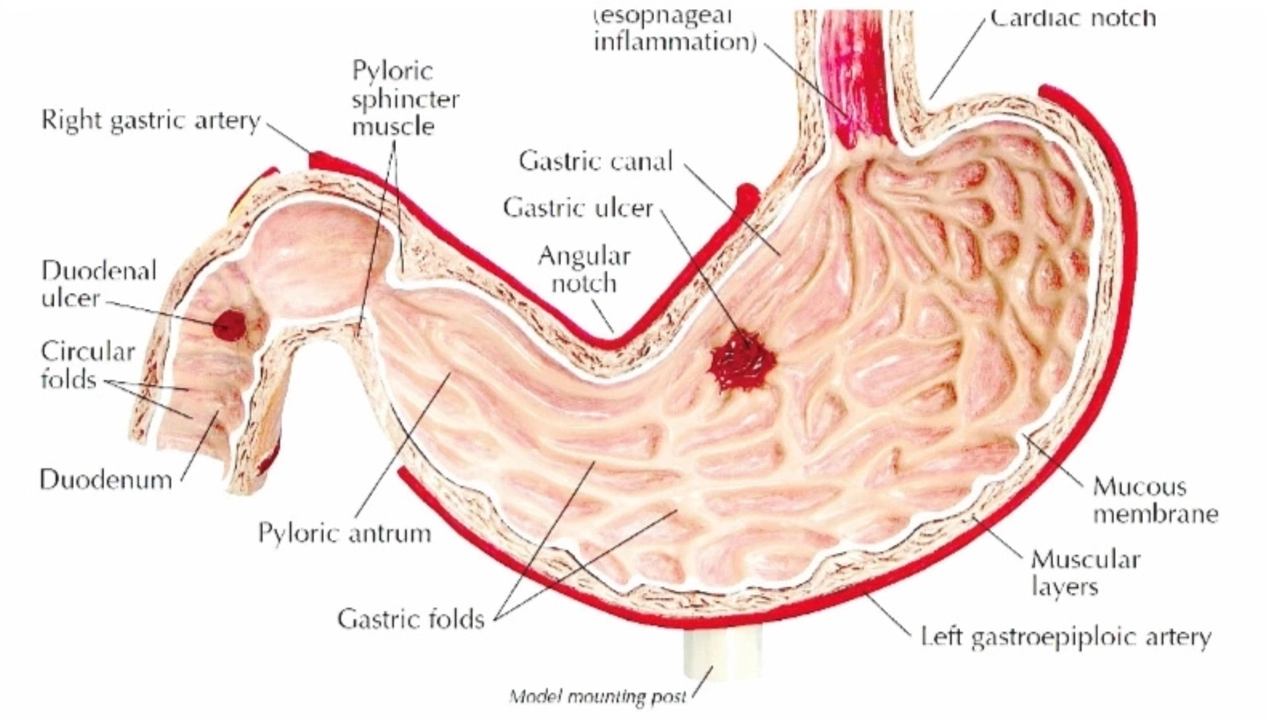
Feeling a burning or gnawing pain in your upper belly after meals or at night? That’s one of the most common signs of a stomach (peptic) ulcer. Ulcers are breaks in the lining of the stomach or the first part of the small intestine. They can be painful, but many people get better once the cause is treated.
What usually causes ulcers
Two causes account for most ulcers. First, an infection with Helicobacter pylori (H. pylori). This bacteria weakens the protective layer of the stomach and allows acid to damage tissue. Second, regular use of NSAIDs — think ibuprofen, naproxen — can irritate and thin the stomach lining. Less often, smoking, heavy alcohol use, or long-term stress can make things worse, but they rarely start ulcers by themselves.
Symptoms can vary. You might feel a dull or burning pain between the breastbone and belly button, often worse when hungry or at night. Other signs include bloating, belching, nausea, reduced appetite, or unexpected weight loss. If you vomit blood or notice black, tarry stools, get medical help right away.
How doctors find and treat ulcers
Diagnosis often starts with a breath or stool test for H. pylori. If those are unclear or symptoms are severe, your doctor may recommend an upper endoscopy to look directly at the stomach lining. Treatment depends on the cause. If H. pylori is present, a short course of antibiotics plus a proton pump inhibitor (PPI) like omeprazole is the usual plan. If NSAIDs caused the ulcer, stopping them and using a PPI or H2 blocker can allow healing.
PPIs reduce stomach acid and help the lining heal. Many people feel better within days, but it’s important to finish the full treatment your doctor prescribes. If you can’t take common antibiotics due to allergy or resistance, there are alternative regimens—your clinician will pick the safest option for you.
Simple self-care helps too. Stop NSAIDs if possible or talk to your doctor about safer pain options. Cut back on alcohol and quit smoking — both slow healing. Eat regular meals, avoid frequent heavy or greasy foods that trigger discomfort, and sleep with smaller, later dinners if night pain is a problem.
If you have recurring ulcers or need long-term NSAIDs, your doctor might suggest a protective medication like a PPI to prevent new ulcers. Follow-up testing to confirm H. pylori is gone is common after treatment.
Ulcers can heal well with the right plan. Watch for worsening pain, vomiting, fainting, or bloody stools — those require immediate care. If your stomach pain just won’t quit, get checked; catching and treating ulcers early keeps things simple and safer.