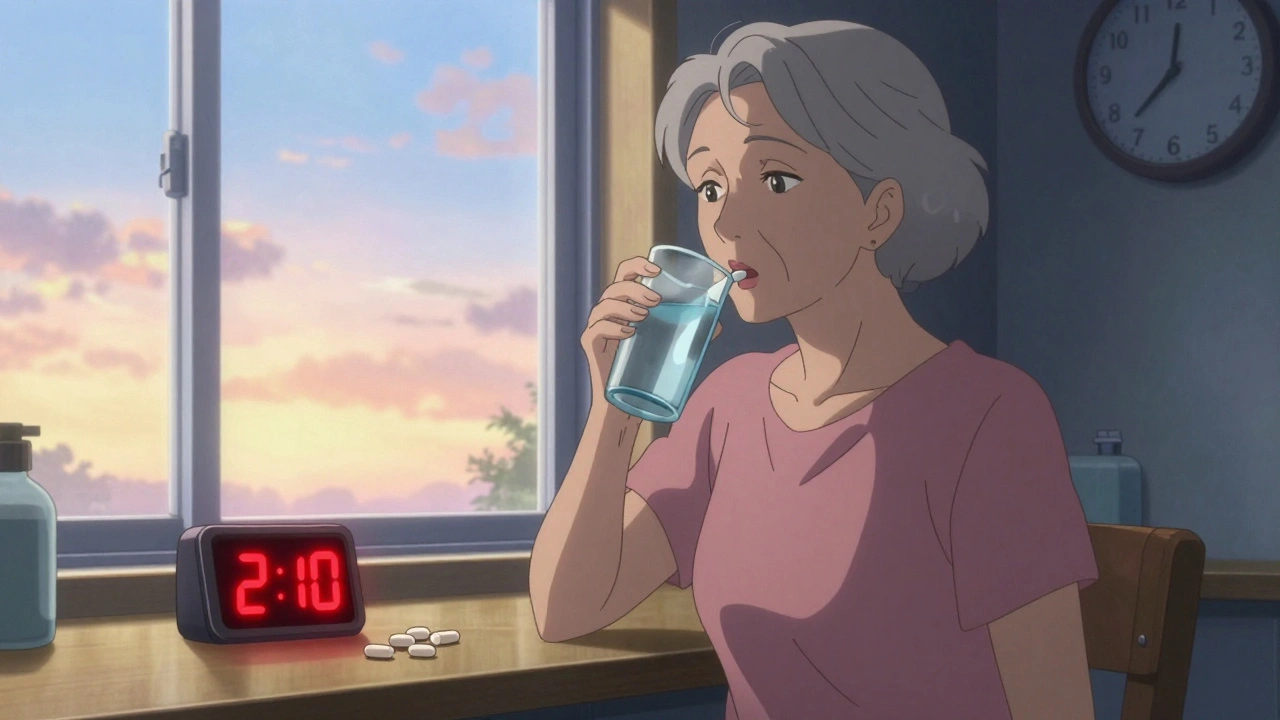
Timing Rules: When to Take Medication for Maximum Effect
When you take a pill isn’t just a habit—it’s part of how it works. Timing rules, the science behind when medications should be taken to match your body’s rhythms and avoid harmful interactions. Also known as dosing schedules, these rules affect everything from how well a drug works to whether it causes nausea, dizziness, or worse. Take blood pressure meds at night? Some studies show they lower morning spikes better than morning doses. Take antibiotics with food? That could kill their effectiveness. Timing rules aren’t arbitrary—they’re built into how your body absorbs, breaks down, and uses medicine.
Drug interactions, when two or more medications interfere with each other’s action, often depend on timing. For example, clopidogrel and omeprazole shouldn’t be taken together because omeprazole blocks the enzyme that turns clopidogrel into its active form. But if you space them out—say, take clopidogrel in the morning and omeprazole at night—you might avoid the problem. Same goes for thyroid meds: taking them with coffee, calcium, or iron can block absorption. The fix? Wait 30 to 60 minutes after taking your thyroid pill before eating or drinking anything but water.
Pharmacokinetics, how your body moves a drug through absorption, distribution, metabolism, and elimination explains why timing matters. Some drugs work best on an empty stomach because food slows them down. Others need food to reduce stomach upset or help absorption. Gabapentin and pregabalin? They’re absorbed faster on an empty stomach, but many people take them with food to avoid dizziness. That’s a trade-off—and it’s why your pharmacist asks if you eat before taking your meds. Even something as simple as taking a diuretic too late in the day can ruin your sleep with midnight bathroom trips.
Timing rules also protect you from overdose risks. Take acetaminophen every 4 hours? That’s safe. Take it every 2 hours because you’re still in pain? That’s how liver damage starts. Same with opioids—taking them too close together can slow your breathing to dangerous levels. The FDA’s serious adverse event reports are full of cases where people didn’t realize timing was the problem.
And it’s not just pills. Glaucoma drops like timolol need to be taken at the same time every day because their pressure-lowering effect fades after 12 to 24 hours. Miss a dose? Eye pressure creeps up. Take it too early? You might wake up with blurry vision. Even supplements like magnesium or vitamin D have optimal times—magnesium before bed helps sleep, vitamin D with breakfast helps absorption.
There’s no one-size-fits-all schedule. Your doctor’s instructions are the starting point, but your body’s response is the real guide. If a medication makes you sleepy, take it at night. If it gives you stomach pain, take it with food. If you’re on five different pills, write down when each one goes in—and why. You’ll spot patterns. You’ll catch conflicts. You’ll avoid surprises.
Below, you’ll find real-world examples of how timing rules affect everyday medications—from antibiotics and blood thinners to glaucoma drops and pain relievers. These aren’t theory pages. They’re stories from patients, pharmacists, and doctors who’ve seen what happens when timing gets ignored—and how getting it right changes everything.