Bisphosphonates: What They Are, How They Work, and What You Need to Know
When your bones start losing density, bisphosphonates, a class of drugs designed to slow bone breakdown and reduce fracture risk. Also known as bone-resorption inhibitors, they’re among the most prescribed treatments for osteoporosis and other conditions that weaken bone structure. These medications don’t rebuild bone, but they stop it from crumbling too fast—giving your body time to maintain what’s left.
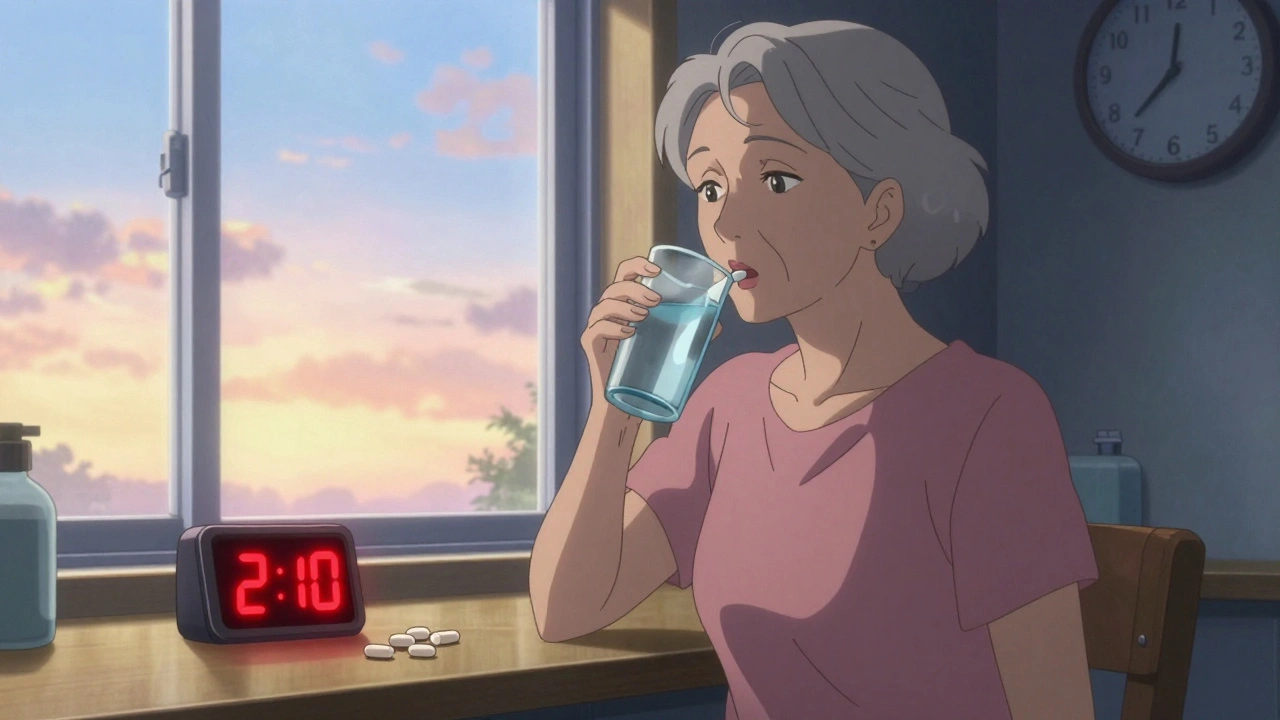
Bisphosphonates are closely tied to osteoporosis, a condition where bones become porous and fragile, often without symptoms until a fracture happens. They’re also used in cases of bone metastases, Paget’s disease, and even in some cancer patients to prevent skeletal complications. But they’re not magic pills. Their effectiveness depends on how long you take them, whether you follow dosing rules (like staying upright after swallowing), and if you’re getting enough calcium and vitamin D. Many people don’t realize that skipping doses or lying down too soon after taking them can make them useless—or worse, irritate the esophagus.
Side effects are real. Some people get heartburn, muscle pain, or jaw problems. A rare but serious risk is osteonecrosis of the jaw, especially after dental work. There’s also a small chance of unusual thigh fractures after long-term use. That’s why doctors don’t hand them out like candy—they weigh your fracture risk against the downsides. If you’ve been on bisphosphonates for more than five years, your provider might suggest a "drug holiday" to let your body reset.
These drugs don’t work the same for everyone. Some people feel better right away. Others notice no change until they break a bone they thought they’d never break. And while they’re often the first choice, they’re not the only option. Alternatives like denosumab or teriparatide exist for those who can’t tolerate bisphosphonates or need something stronger.
What you’ll find below is a collection of real-world posts that dig into the details you won’t get from a pamphlet. You’ll see how bisphosphonates compare to other bone drugs, what the latest safety data says, how they interact with other meds, and why some people stop taking them—even when their doctor says to keep going. There’s also practical advice on how to take them safely, what to ask your pharmacist, and how to spot warning signs before they become emergencies. This isn’t theory. It’s what patients and providers are dealing with right now.